Pancreatic beta cell (islet) transplantation is carried out as a curative treatment method for diabetes, but to prevent rejection, patients have to use immunosuppressants for the rest of their lives after the transplant. Professor Emeritus Yohichi Yasunami of the Research Institute for Islet Biology, Fukuoka University Central Research Organization, Fukuoka University, and his colleagues have been engaged in developing a subcutaneous adipose tissue transplantation method for the transplantation of pancreatic beta cells into subcutaneous fat rather than the liver and have now clarified that it is possible to prevent rejection by adding bFGF (basic fibroblast growth factor) treatment. Professor Emeritus Yasunami noted, "In the future, we want to develop this for humans after verifying it in primates such as cynomolguses." Their outcomes were published in the electronic version of Diabetes, the journal of the American Diabetes Association.
There are around 20 million diabetes patients in Japan, and it is believed that 100,000 to 200,000 of these people suffer serious illness and must continue to have insulin injections throughout their lives. One method of freeing patients from insulin injections that has attracted attention is islet cell transplantation, which transplants islet cells that create insulin into patients. However, to ensure that the transplanted cells engraft after the transplant and have a curative effect, it is necessary to prevent rejection of the transplanted cells. Immunosuppressants are used for this, and post-transplant diabetes patients must take these for the rest of their lives. On the other hand, the reduced immunity caused by the immunosuppressants has the secondary effect of increasing the risk of infectious diseases and malignant tumors, so people have hoped for the development of a method to prevent rejection that would, ideally, not use immunosuppressants. Notably, immunosuppressants can have the secondary effect of causing developmental disorders in infants with type 1 diabetes and so cannot be used. At the present time, islet transplantation is not carried out for infants with type 1 diabetes.
The current treatment method involves transplanting pancreatic beta cells into the liver, but one major issue with the liver is characteristic early-stage rejection, so the engraftment ratio was low. However, Professor Emeritus Yasunami and his colleagues have developed and reported a subcutaneous adipose tissue islet transplantation method that greatly improves the engraftment ratio by using subcutaneous fat as the transplant site of the pancreatic beta cells. Now, they have further improved this by developing a method to control rejection without using immunosuppressants.
This research made use of an experimental system involving mouse islet transplantation. When islets isolated from white mice (BALB/c) were transplanted into the subcutaneous adipose tissue in the groin area of diabetic black mice, the hyperglycemia of the black mice temporarily normalized thanks to the insulin secreted by the transplanted islets. However, the transplanted islets were destroyed due to rejection around 10 days after the transplant, the insulin dried up, and the black mice once again became hyperglycemic.
For this experimental system, agarose rods containing a drug (bFGF) were placed in the recipients' subcutaneous adipose tissue two weeks before the transplant. When islets were transplanted in these sites, the blood sugar of the diabetic mice was normal for a long period of time after the transplant (around a year), without any hyperglycemia. One year after the transplant, subcutaneous adipose tissue, including the islets that had been transplanted, was removed, and the recipients became hyperglycemic. This outcome indicates that the normal blood sugar of the recipients was caused by the insulin secreted by the transplanted islets.
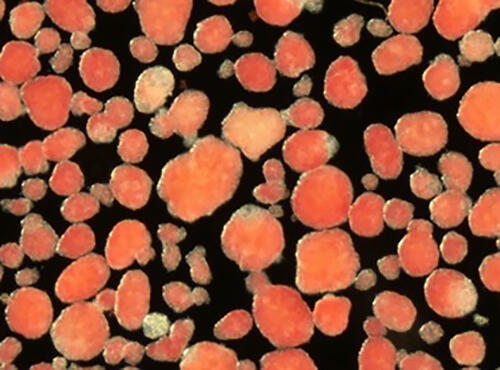
Normal transplanted islets were confirmed in microscopic observation of the extracted tissue, proving that the transplanted islets had engrafted without being rejected for over a year, without the use of immunosuppressants. The lifespan of a mouse is slightly over a year, so the fact that the transplanted islets engrafted for over a year through the rejection prevention method developed by the group means that this method was able to prevent rejection without immunosuppressants for a lifetime.
The pretreatment led to the induction of large quantities of mesenchymal stem cells that produce TGFβ, an immunosuppressive factor, in the subcutaneous adipose tissue. In addition, the group learned through another experiment that if the mesenchymal stem cells induced in the subcutaneous adipose tissue by the pretreatment are isolated and transplanted into a diabetic mouse together with isolated islet cells, the transplanted islet cells engraft without immunosuppressants. This clarified that the TGFβ-producing mesenchymal stem cells transplanted with these are limited to the transplant site and prevent rejection over a long period of time.
In the future, it is hoped that if researchers create pancreatic beta cells from iPS cells and carry out transplant surgery, they will realize a procedure that avoids rejection by transplanting these with TGFβ-producing mesenchymal stem cells.
Provided by Professor Emeritus Yohichi Yasunami, Fukuoka University
Journal Information
Publication: Diabetes
Title: Acceptance of Murine Islet Allografts Without Immunosuppression in the Inguinal Subcutaneous White Adipose Tissue Pretreated with bFGF
DOI: 10.2337/db21-0684
This article has been translated by JST with permission from The Science News Ltd.(https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




