Director General Junichi Nabekura of the National Institute for Physiological Sciences, Assistant Professor Ikuko Takeda of the Department of Anatomy and Molecular Cell Biology in the Graduate School of Medicine at Nagoya University, Professor Makoto Tsuda of the Graduate School of Pharmaceutical Sciences at Kyushu University, Professor Koizumi Shuichi of the Department of Neuropharmacology at the University of Yamanashi, and lecturer Kei Eto of the School of Allied Health Services at Kitasato University have clarified a new treatment strategy for neuropathic pain.
Provided by the National Institute for Physiological Sciences
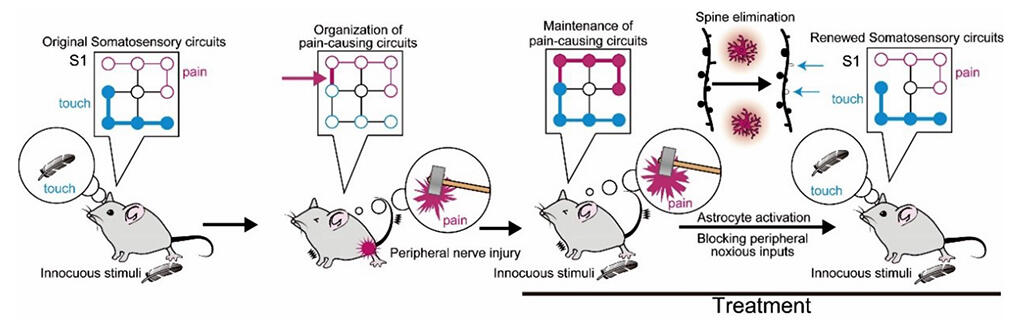
Chronic pain is an intractable condition in which hyperalgesia, the sensation in which pain is felt even through touch, persists for an extended period of time. The research group had previously reported, via the use of pathological mouse models, that one of the causes is a pathological circuit that is created in the somatosensory region of the cerebral cortex, which receives sensory information such as pain and touch.
In an attempt to restore this pathological circuit to normal, the research group focused on astrocytes (a type of glial cell in the brain) that are responsible for recombining neural circuits during developmental periods. Astrocytes act in the formation and removal of synapses and are considered to be important for recombining neural circuits. In this research, using a neuropathic pain model in mice, astrocytes in the primary somatosensory cortex were artificially activated via transcranial direct current stimulation (tDCS) and via DREADD, a type of artificial receptor, while pain input from the peripheral nerves was temporarily suppressed via drugs.
The results confirmed that the pain-relieving effects persisted not only during the treatment, but also for an extended period of time after the treatment. When the research group investigated the mechanism of action from the viewpoint of neural circuits, it became clear that the activation of astrocytes removes the spines that connect neural circuits in the primary somatosensory cortex, and that the spines formed during the onset of pain are particularly susceptible to removal. This suggests that pain-related spines are removed, and pain-related circuit reorganization occurs when the astrocytes are activated while pain input is suppressed.
According to Director General Nabekura, "In order to find a way to apply this technology to clinical medicine, we held discussions with neurologists and confirmed that tDCS, which is used in clinical medicine, can activate cortical astrocytes in mice. We can expect more effective treatments by combining tDCS and local anesthesia of peripheral sensory nerves, two methods that are already used for treatment."
This article has been translated by JST with permission from The Science News Ltd.(https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.