A research group led by graduate student Ai Yaku and Professor Osamu Takeuchi of the Graduate School of Medicine, Kyoto University, along with Director Yoshikazu Nakaoka of the Department of Cardiovascular Medicine, National Cerebral and Cardiovascular Center, announced that they have clarified the pathology of pulmonary arterial hypertension (PAH), an intractable disease. Regnase-1, which suppresses the activation of immune cells, was found to be involved in the onset and severity of the disease. Mice that were lacking in Regnase-1 in their cells, including alveolar macrophage (some of the most abundant innate immune cells in the lungs), were created during the research process, and these exhibited the pathology of connective tissue disease-PAH. From this it was found that they can be used as model mice. The results are expected to lead to the development of new therapeutic agents for PAH and were published in the August 23 issue of the international scientific journal Circulation.
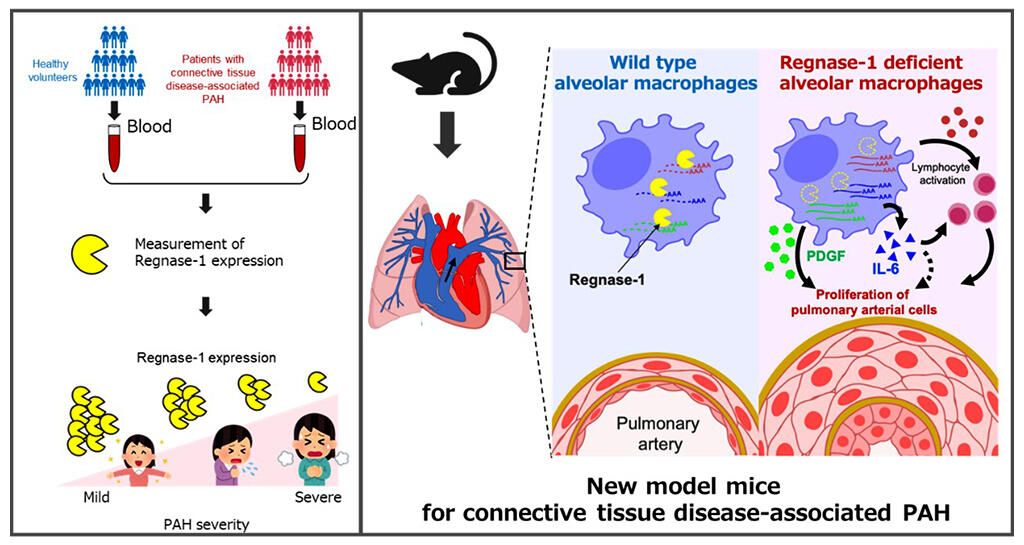
(Right) Proposed mechanism of Regnase-1-mediated PAH inhibition via alveolar macrophages identified by mouse experiments.
Provided by Kyoto University
Pulmonary hypertension is a general term for diseases in which the blood pressure in the pulmonary arteries, which supply blood from the heart to the lungs, becomes too high. It can be caused by a variety of factors, and when heart function declines, the oxygen supply to the whole body is reduced. As it progresses, individuals may experience shortness of breath, and the disease can lead to death due to right heart failure. PAH is caused by a thickening of the wall of the pulmonary artery and a narrowing of the lumen, with typical examples including idiopathic (unknown cause) PAH and connective tissue disease-PAH that is associated with connective tissue diseases. In particular, connective tissue disease-PAH is known to have a poorer prognosis than other types of pulmonary hypertension because it is often accompanied by intractable conditions such as pulmonary vein occlusion and cardiac fibrosis. Current PAH therapies are aimed at vasodilation but have limited therapeutic effects, and, although patients' blood have high levels of inflammatory cytokines, it was not known which cells were producing the inflammatory cytokines and there were also no model mice.
From this background the research group focused on Regnase-1, which acts as a brake that suppresses immune cell activation and inflammation. Regnase-1 is an enzyme that degrades the mRNA encoding proteins involved in immune cell activation, including inflammatory cytokines such as IL-6, and suppresses immune responses.
First, the expression levels of the Regnase-1 gene in the blood cells of pulmonary hypertension patients and healthy subjects were compared. The results showed that the expression level was significantly lower in patients with pulmonary hypertension. Furthermore, when the event survival rates of the patients were compared according to their level of Regnase-1 expression, the lower group had a significantly worse prognosis for the disease. When PAH patients were examined in the same manner, it was found that Regnase-1 expression was negatively correlated with disease severity, especially in patients with collagenous PAH.
Based on these results, to verify the function of Regnase-1 the research group created two mouse lines that are deficient in Regnase-1 in myeloid cells that produce inflammatory cytokines.
Both strains of mice spontaneously developed PAH and showed pulmonary artery plexiform lesions that were difficult to reproduce in existing PAH model mice, and were complicated by the pulmonary vein occlusion and cardiac fibrosis in connective tissue disease-PAH. As such, the research group believes that these mice can be used as a model to reproduce connective tissue disease-PAH. The two strains of mice also shared a common Regnase-1 deficiency in alveolar macrophages, which may be responsible for connective tissue disease-PAH.
When these mice were treated with a drug that eliminated alveolar macrophages, their PAH condition improved. As a result, it became clear that Regnase-1 in alveolar macrophages regulates the pathogenesis of PAH. The research group has also identified a gene that causes abnormal proliferation of pulmonary artery constituent cells, which is regulated by Regnase-1.
Journal Information
Publication: Circulation
Title: Regnase-1 Prevents Pulmonary Arterial Hypertension Through mRNA Degradation of Interleukin-6 and Platelet-Derived Growth Factor in Alveolar Macrophages.
DOI: 10.1161/CIRCULATIONAHA.122.059435
This article has been translated by JST with permission from The Science News Ltd.(https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




