Professor Ai Kotani, Specially Appointed Assistant Professor Yuji Miyatake, Graduate Student Kazuaki Kameda (at the time of the study), and Research Fellow Ryou Yanagiya from the Department of Advanced Medical Science at Tokai University School of Medicine along with Perseus Proteomics Inc. (PPMX) performed a joint study showing that aggressive NK-cell leukemia (ANKL) proliferates in the sinusoids of the liver and is dependent on the interaction between the iron-carrying protein transferrin (Tf) and its binding partner transferrin receptor 1 (TfR1). They also observed that the TfR1-targeting antibody PPMX-T003 had marked antitumor activity against ANKL. Physician-initiated clinical trials of PPMX-T003 in patients with ANKL are scheduled to start during this fiscal year. These results were published in the online edition of the journal Blood.
Provided by Tokai University
ANKL is a hematological cancer that develops at a young age, with an extremely poor prognosis and a median survival time of less than 2 months from onset. It is a rare disease with an average annual incidence of 10 people in Japan and no standard treatment has yet been established.
Extending patient survival requires prompt allogeneic hematopoietic stem cell transplantation. Its efficacy requires a sufficient reduction in the numbers of cancer cells prior to transplantation. At present, L-asparaginase is the only anticancer drug that is relatively effective against ANKL; however, it sometimes causes serious liver damage. Many patients with ANKL also have severe liver damage caused by the cancer cells and cannot tolerate the high doses required for treatment. In such cases, either the drug must be discontinued, or the dosage must be reduced. However, low doses might not sufficiently target and reduce cancer cells.
To successfully treat the disease, the liver damage caused by ANKL must be overcome. This means that both testing of cancer cells grown in culture medium and also determination of how the cancer cells survive and proliferate in the liver is required.
To this end, the research group transplanted cancer cells collected from three patients with ANKL into immunodeficient mice to establish an ANKL-PDX mouse model. Over time, these mice were dissected, and the cancer cells in each organ were analyzed. The analysis revealed that the cancer cells had engrafted and proliferated in the liver in the early stage and later spread to organs throughout the body.
Microscopic observation of the cancer cells in the liver revealed that they proliferated in the sinusoids (capillaries) that carry nutrients and minerals into and out of the liver. Based on these observations, they thought that ANKL proliferation was dependent on some substance that is exchanged in the liver.
They comprehensively examined the molecules that are expressed and secreted by the cancer cells and surrounding liver cells using next-generation sequencing and then searched for pairs that may bind or be exchanged.
A pair, consisting of liver cell-expressed Tf and ANKL cell-expressed Tf receptor (TfR1), which binds Tf, was the top hit. Tf is a protein that transports iron ions, and it is taken up by cells mainly through binding to TfR1. As Tf is abundant in the liver, one of the reasons why ANKL cancer cells proliferate in the liver sinusoids may be to obtain iron ions via the Tf/TfR1 pair.
It was confirmed that receiving Tf from the liver side enabled proliferation. In ANKL-PDX mice carrying a TfR1 knockout, which is expressed on ANKL cancer cells, the proliferative activity of the cancer cells in the liver was substantially reduced. This confirmed that Tf from the liver promotes ANKL proliferation.
The researchers then approached PPMX Ltd., a company that had developed an inhibitory antibody against TfR1, and they jointly conducted a study to test if the TfR1 inhibitory antibody PPMX-T003 could be an effective therapeutic agent for ANKL. Cancer cells derived from three patients with ANKL were cultured in medium containing PPMX-T003 for 48 h, and then the number of viable cells was counted. The researchers observed that the viability of the cancer cells decreased depending on the concentration of PPMX-T003.
Next, a single dose of PPMX-T003 was administered to PDX mice on the 7th day after model establishment, and cancer cell proliferation was evaluated 1 week later by observing the ratio of cancer cells to leukocytes. The results showed that the proliferative ability of the cancer cells was markedly decreased when PPMX-T003 doses of 3 mg/kg or higher were administered.
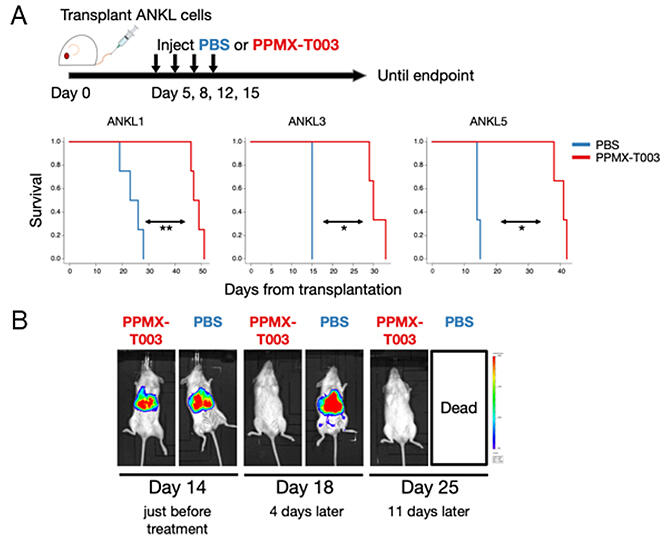
Finally, to mimic the actual treatment scenario, the inhibitor was administered intravenously to ANKL-PDX mice multiple times to examine whether there was a difference in survival time. The results showed that survival was extended by 1.5 to 2 times. This prolongation effect was also observed after administering the inhibitor to ANKL-PDX mice with more advanced symptoms (at 14 days after model establishment).
Then, they quantified the change in the amount of cancer cells in the liver before and after treatment using mice with luminescent (or glowing) cancer cells. Before treatment, significant luminescence was observed in the liver region. However, after treatment, the luminescence quickly disappeared.
Based on these results, the research group aims to start an investigator-initiated clinical trial (Phase Ib/II trial) in 2023 to study the efficacy and safety of the inhibitor (PPMX-T003) in patients with ANKL at Tokai University, Tohoku University, Okayama University, Kyoto University, Kyushu University, and Hiroshima University. The clinical trial will proceed without delay, and in the future, the pathophysiology related to the strong iron dependence of ANKL will be further analyzed.
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




