A research group led by Visiting Professor Tomohiro Watanabe of the Department of Gastroenterology and Hepatology at the Faculty of Medicine and Graduate Student Yasuo Otsuka of the Faculty of Medicine at Kindai University revealed that intracellular leucine-rich repeat kinase 2 (LRRK2) activation due to the inflammatory response induced by fungal infection is involved in the development of severe acute pancreatitis. The study results were published in the journal Clinical & Experimental Immunology.
Provided by Kindai University
The number of patients with acute pancreatitis is increasing (78,000 in 2016). The proportion of patients who develop a severe condition is 19.7%, with death occurring in approximately 20% of such cases. Although alcohol and a high-fat diet are known to lead to acute pancreatitis progression by activating trypsinogen in pancreatic acinar cells, which leads to excessive production of the digestive enzyme trypsin and autolysis (cellular self-digestion), the detailed molecular mechanism is unknown, and no radical treatment option is available. Moreover, the discovery that mice with no pancreatic enzymes can also develop pancreatitis suggests that another pathogenic mechanism exists. Before the current study, the research group had determined that pancreatitis is worsened by the immune response to the gut bacteriome that occurs via nucleotide-binding oligomerization domain-containing protein 1 (NOD1).
Otsuka said, "30% to 40% of patients with severe acute pancreatitis have concurrent fungal infections, and the mortality rate of those patients is reported to be 40%. We targeted LRRK2, a protein associated with Parkinson's disease, because it is said to be involved in the immune response to fungi."
In the current study, administering LRRK2 inhibitors to mice with drug-induced acute pancreatitis prevented immune cell infiltration into the pancreas, reduced inflammatory cytokine production, and inhibited pancreatitis. Additionally, administering the drug to induce acute pancreatitis in LRRK2-overexpressing mice worsened the condition. In the LRRK2-overexpressing mice, increased macrophage infiltration into the pancreas and inflammatory cytokine production were observed. At the same time, LRRK2 expression was observed both in pancreatitis-associated pancreatic acinar cells and in immune cells.
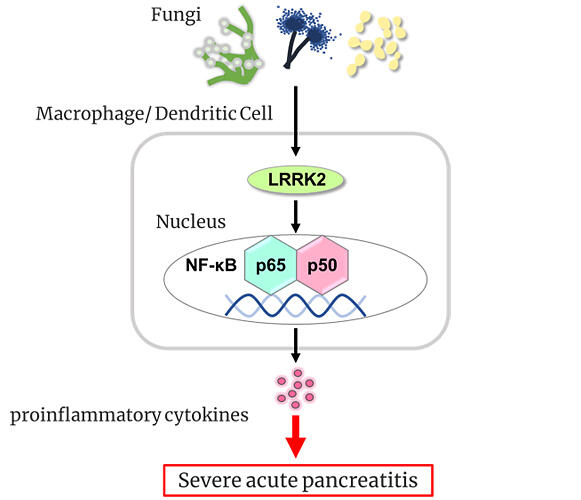
The research group further generated mice that overexpressed LRRK2 in immune cells only. When acute pancreatitis was induced, the condition worsened, indicating that immune cells were involved in the worsening effect. LRRK2 activates nuclear factor-kappa B (a transcription factor) to increase inflammatory cytokines interleukin (IL)-6, TNF-αtumor necrosis factor-alpha, and IL-12/23p40 production, contributing to severe pancreatitis.
This raised the question of what activates LRRK2. Elimination of the gut bacteriome in LRRK2-overexpressing mice by administering water containing antibacterial drugs to the animals did not inhibit pancreatitis. By contrast, administering water containing antifungal drugs to the animals eliminated the gut fungal mycobiome in the mice, thus inhibiting pancreatitis and markedly decreasing the levels of inflammatory cytokines.
Watanabe stated, "First, acute pancreatitis impairs the pancreatic barrier. Then, when the gut fungal mycobiome enters the pancreas, immune cells recognize it and activate LRRK2. We think that activated LRRK2 causes the development of severe pancreatitis by inducing inflammatory cytokine production."
The current study proposes that controlling LRRK2 function or eliminating the gut fungal mycobiome could be novel therapeutic approaches for alleviating acute pancreatitis. LRRK2 inhibitors are currently being tested in clinical trials for the treatment of Parkinson's disease.
Watanabe added, "Quantifying LRRK2 itself is difficult, but its genetic mutation is known to cause various conditions, including Parkinson's disease, Crohn's disease, and leprosy. The risk of developing a severe condition may be estimated through genome sequencing of the blood cells. Based on the estimated risk, it may be possible to prevent severe conditions using inhibitory agents."
Journal Information
Publication: Clinical & Experimental Immunology
Title: Leucine-rich repeat kinase 2 promotes the development of experimental severe acute pancreatitis
DOI: 10.1093/cei/uxad106
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




