Using a mouse model, a research group at Tohoku University and collaborating institutions has announced that they have discovered that stimulating the vagus nerve, which connects the brain and pancreas, increases the number of cells that produce insulin, a hormone that lowers blood sugar. This discovery is expected to facilitate the development of methods for treating and preventing diabetes caused by elevated blood sugar.
Diabetes is frequently caused by a decrease in the number or function of the pancreatic beta cells that produce insulin, resulting in decreased insulin and increased blood sugar levels. Diabetes treatments include the injection of insulin to supplement the body's production. A therapeutic approach that increases the number of beta cells is expected, but it has not yet been developed.
In obese individuals, however, the number of beta cells increases, and more insulin is produced to suppress the increase in blood sugar levels. Although the mechanism remains unknown, the research group previously found that signals from the vagus nerve have an important effect on beta cells. Due to this, they thought that stimulating the vagus nerve, which connects to the pancreas, could increase the number of beta cells and treat diabetes, and conducted experiments using optogenetic techniques.
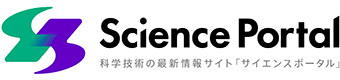
They created genetically modified mice whose vagus nerves were activated when exposed to blue light. Particles that glowed blue upon exposure to near-infrared light, which can penetrate living organisms, were injected into the pancreas. The mice were exposed to near-infrared light from outside the body, stimulating the vagus nerve that connects to the pancreas to activate the beta cells to produce more insulin. This is the first study to control nerves in a peripheral organ using optogenetic stimulation.
Provided by Tohoku University
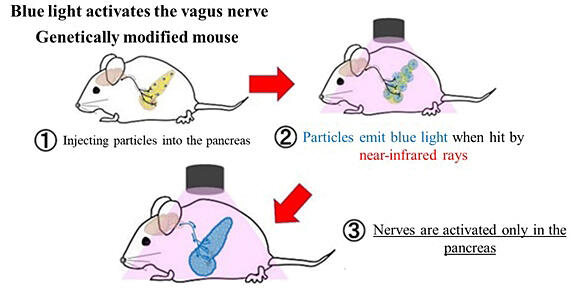
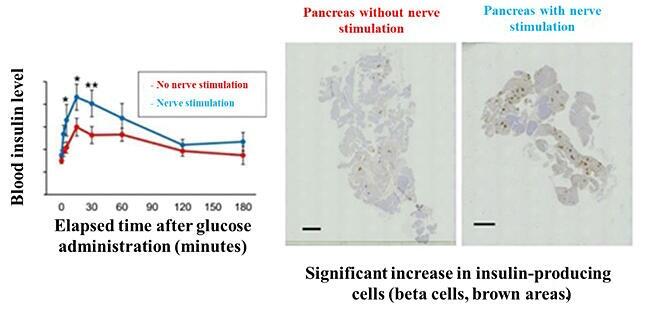
In a mouse model of diabetes, the vagus nerve connecting to the pancreas was stimulated, which significantly increased insulin levels and activated beta cells in response to sugar administration. After continuous stimulation for approximately 2 weeks, the number of beta cells more than doubled. This method was used to suppress the increase in blood sugar levels and successfully treat diabetes in mice for the first time.
(Left) Insulin levels increased after sugar was administered than when no stimulation was applied; (Right) Beta cells of pancreas (brown areas) increased.
Provided by Tohoku University
Provided by Tohoku University
Similar genetic modifications are not feasible in humans. However, epilepsy, depression, and some types of enteritis are surgically treated in humans by attaching electrodes to the vagus nerve and applying electrical stimulation. The research group believes that similar stimulation of the vagus nerve connecting to the pancreas may lead to diabetes prevention and treatment in humans.
At a press conference, Associate Professor Junta Imai of the Endocrine and Metabolism Division, Department of Diabetes and Metabolism, Graduate School of Medicine at Tohoku University said, "I am expecting that this result will lead to the development of unprecedented diabetes prevention and treatment methods, and I have started some clinical research in this topic. Examining the function of the vagus nerve will help us to elucidate the cause and pathology of diabetes. We achieved a very important result."
The research group consists of Tohoku University, Tohoku Medical and Pharmaceutical University, Tokyo Medical and Dental University, and Nagoya University. The results were published on November 10th in the British medical bioengineering journal Nature Biomedical Engineering. The research was supported by the Ministry of Education, Culture, Sports, Science and Technology's Grant-in-Aid for Scientific Research, the Japan Science and Technology Agency Moonshot R&D Project, and the Japan Agency for Medical Research and Development Innovative Advanced Research and Development Support Project.

Original article was provided by the Science Portal and has been translated by Science Japan.