A research group led by Professor Hidetoshi Hayashi of Kindai University Faculty of Medicine, Specially Appointed Professor Kazuhiko Nakagawa of Kindai University Hospital Cancer Center, Professor Kenji Chamoto of Kyoto University Graduate School of Medicine, and Distinguished Professor Tasuku Honjo of Kyoto University Institute for Advanced Study in collaboration with Sysmex Corporation (President Kaoru Asano) announced their results showing that the therapeutic effects of anti-PD-1 antibodies such as Opdivo against non-small-cell lung cancer (NSCLC) can be predicted from "immune checkpoint factors" in the blood. The findings are expected to contribute to the provision of more effective treatment and the reduction of healthcare costs and were published in the April 2 issue of the Journal of Clinical Investigation.
Provided by Kindai University
Lung cancer includes NSCLC and small-cell lung cancer (SCLC), with the former accounting for about 80% of cases. Stage 4 NSCLC had a very low 5-year survival rate of 1%−2% until the 1990s. With the development of new drugs, the survival rate has increased to about 20% since the 2000s. After immune checkpoint inhibitors (anti-PD-1 antibodies) became available for use in clinical practice in 2015, the survival rate has further increased and remission has been achieved in some cases, although the survival rate is still not high.
Immune checkpoint inhibitors work by inhibiting PD-1 (an immune checkpoint protein), which was previously discovered to exist on the surface of immune cells by Honjo. Anti-PD-1 antibodies enhance the immune response and exert antitumor effects by inhibiting the binding of PD-1 to PD-L1 produced by cancer cells. Meanwhile, immune checkpoint inhibitors provide long-term efficacy in approximately 10%−20% of patients. It was a challenge to predict the type of patients for whom the inhibitors are effective.
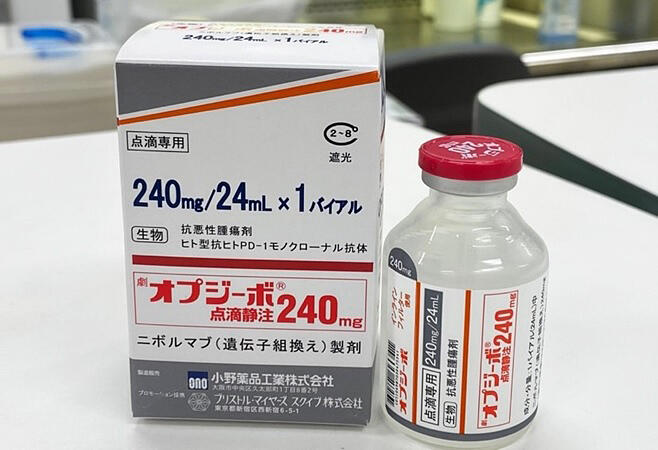
Since 2015, Kindai University, Kyoto University, Ono Pharmaceutical, and Sysmex have been conducting the "Nivolution trial," a physician-led clinical trial to search for biomarkers of anti-PD-1 antibodies in patients with advanced NSCLC. Blood samples were collected from 50 patients before they were treated with Opdivo. Soluble immune checkpoint factors (sPD-L1, sPD-1, and sCTLA-4) were measured using Sysmex's fully automated immunoassay system, HISCL. The device can measure various biomarkers, such as proteins, in trace amounts (approximately 10−30 µ-liter) of blood with high sensitivity in a short time, and the company has been constructing a measurement system for these factors which are expressed on lymphocytes and other cells, and some of them are known to be suspended and circulated in the blood.
In the present study, they analyzed the relationship between these factors and the therapeutic effect of Opdivo. The results on the 12-month progression-free survival rate showed that efficacy was higher in patients with a lower level of sPD-L1 or sCTLA-4 and even higher in patients with lower sPD-L1 and sCTLA-4 levels. The relationship between soluble immune checkpoint factors and PD-L1 expression in tumor tissue (as assessed by immunostaining) was examined, and the results showed that the predictive ability of immunostaining, which is already used as a biomarker, was complemented and improved by the soluble immune checkpoint factor levels. As an additional study, 147 patients treated with anti-PD-1 and anti-PD-L1 antibodies at Kindai University Hospital, Kyoto University Hospital, and Izumi City General Hospital were analyzed. They confirmed that soluble immune checkpoint factors can predict high efficacy. No associations with the efficacy of anticancer drugs or molecular targeted drugs were found, indicating that soluble immune checkpoint factors are specific biomarkers for immune checkpoint inhibitors. Analysis of tumor size, tumor tissue PD-L1 expression, and gene expression in tumor tissue and peripheral blood CD8+ T cells also showed higher gene expression of immune exhaustion fatigue factors in T cells from patients with higher concentrations of soluble immune checkpoint factors.
Journal Information
Publication: Journal of Clinical Investigation
Title: Soluble immune checkpoint factors reflect exhaustion of antitumor immunity and response to PD-1 blockade
DOI: 10.1172/JCI168318
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




