A research group led by Professor Shinji Tanaka and Assistant Professor Shu Shimada from the Department of Molecular Oncology, Graduate School of Medical and Dental Sciences at the Institute of Science Tokyo and Collaborative Researcher Tomohiko Taniai of the Division of Gene Therapy, Research Center for Medical Sciences at the Jikei University School of Medicine has announced that liver cancers can be classified into subtypes through single-cell analysis of approximately 700 cases. They confirmed that combination therapy with angiogenesis inhibitors and immune checkpoint inhibitors is effective for high-grade MTM/VECT liver cancer. The effectiveness of this combination therapy was also verified in mice. These findings are expected to lead to new liver cancer treatment strategies. The results were published in the February 26 issue of the journal of the American Association for the Study of Liver Diseases, Hepatology.
Provided by Science Tokyo
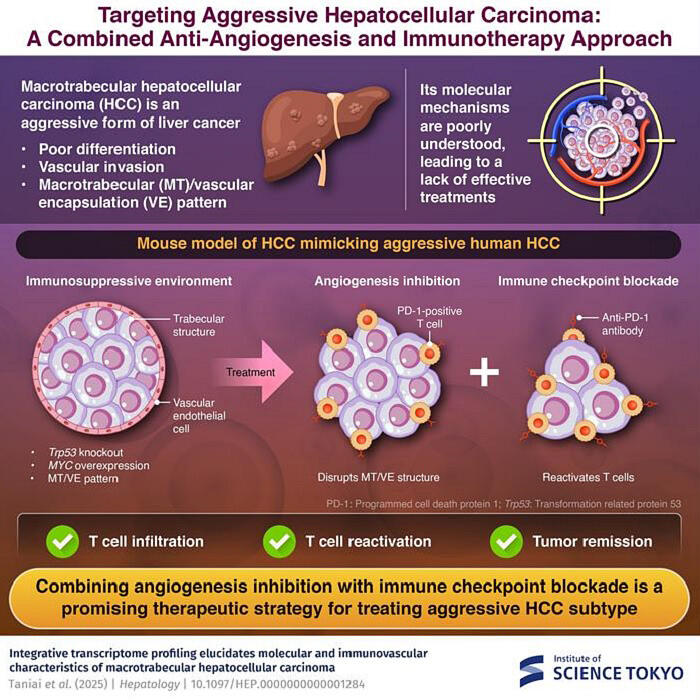
Liver cancer progresses from various chronic liver diseases. It has frequent recurrences, remains a disease with poor prognosis, and shows significant individual differences, suggesting the need for personalized medicine for more effective treatment. These cancers are classified into "proliferative type," with many having mutations in the TP53 tumor suppressor gene (p53 mutation), and "non-proliferative type." Highly invasive and metastatic high-grade liver cancers with macrotrabecular-massive (MTM) architecture, where cancer cells are stacked in more than 10 layers, or vessels encapsulating tumor clusters (VECT), structures where vascular endothelial cells surround tumor masses, account for 30% of cases. However, the molecular mechanisms underlying these structures were previously unknown.
To more accurately classify liver cancer subtypes, the research group conducted bulk analysis using all cells constituting tumors and single-cell analysis of liver cancer cells only (228,564 cells) on 691 cases registered in public liver cancer databases and performed integrated analysis using supercomputers. The bulk analysis classified the cancers into three previously reported types: MS1 (high-grade), MS2 (CTNNB1 mutation), and MS3 (metabolic abnormality). Gene pathway analysis revealed that p53/MYC abnormalities play a central role in MS1. Single-cell analysis of approximately 230,000 cells revealed five major clusters: Cluster 1 (enhanced cell division), Cluster 2 (activated Wnt/β-catenin signaling), Cluster 3 (elevated glycolysis), and Clusters 4 and 5 (enhanced lipogenesis). Furthermore, pseudo-bulk analysis showed that MS1 is composed of combinations of Clusters 1, 3, 4, and 5, with decreased T-cell infiltration also confirmed.
When examining specimens with p53/MYC abnormalities corresponding to the MS1 subtype, the group confirmed many MTM/VECT liver cancers with fewer T cells. They also found that this subtype could be predicted by CT imaging.
As a model for high-grade liver cancer, they created mouse liver cancer cells with p53 deficiency and MYC expression. When these cells were subcutaneously transplanted into mice, they reproduced MTM/VECT liver cancer with decreased T-cell infiltration. Initially, T cells were present, but after 3-4 weeks of subcutaneous transplantation, MTM/VECT structures formed and T cells decreased. It was confirmed that immune checkpoint inhibitors were ineffective in the MTM/VECT structural state. When these cell lines were transplanted into normal immune mice and treated with a combination of an angiogenesis inhibitor (lenvatinib) and an immune checkpoint inhibitor (anti-PD-1 antibody), significant tumor shrinkage was observed. The angiogenesis inhibitor eliminated the MTM/VECT structure, and increased infiltration of T lymphocytes into the tumor was confirmed. The MTM/VECT structure appeared to act as a barrier inhibiting immune cells. There is potential to enhance therapeutic effects by using stronger angiogenesis inhibitors after identifying the subtype.
Tanaka commented, "In the future, we would like to examine data from ongoing clinical trials to assess the effects on different subtypes. While this study focused on MS1, we also want to investigate other subtypes and develop appropriate treatment methods for them."
Journal Information
Publication: Hepatology
Title: Integrative transcriptome profiling elucidates molecular and immunovascular characteristics of macrotrabecular HCC
DOI: 10.1097/HEP.0000000000001284
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




