A research group led by Associate Professor Hirotaka Hamada of the Department of Obstetrics at Tohoku University Hospital, and Graduate Student Hikaru Karumai of the Tohoku University Graduate School of Medicine announced their research results showing that secondhand smoke exposure, as well as maternal smoking during pregnancy, increased the risk for placental abruption. They analyzed the association in data from approximately 80,000 pregnant women and found that about 2.8% and 3% of placental abruption cases can be prevented by abstention from smoking during pregnancy and prevention of secondhand smoke exposure. The findings are expected to lead to the strengthening of anti-smoking measures. The results were published in the international journal BMJ Open on March 4.
Provided by Tohoku University
Toxic chemical components in cigarette smoke have been shown to damage the cells that make up the placenta and reduce blood flow to it from the mother. Smoking during pregnancy has been reported to increase the risk for preterm delivery (<37 weeks), gestational hypertension, and placental abruption, as well as fetal growth restriction, low-birth-weight newborns (<2500 grams), and sudden infant death syndrome.
Under normal circumstances, the placenta detaches after delivery, but placental abruption is a condition in which the normally implanted placenta detaches from the uterus during pregnancy or the course of labor, occurring in about 0.4%-1% of all pregnancies. If placental abruption occurs, the pregnancy must be terminated regardless of the number of weeks of gestation because the placenta that has detached cannot be returned. It is an unpredictable and serious condition, and possible outcomes in severe cases include hysterectomy, maternal death, premature birth, and intrauterine fetal death. Prevention is important because there is no radical treatment.
Maternal smoking during pregnancy (active smoking) has been previously reported to increase the risk of placental abruption. Meanwhile, no previous studies in Japan or other countries have reported relationships between secondhand smoke exposure (passive smoking) and the placental abruption risk.
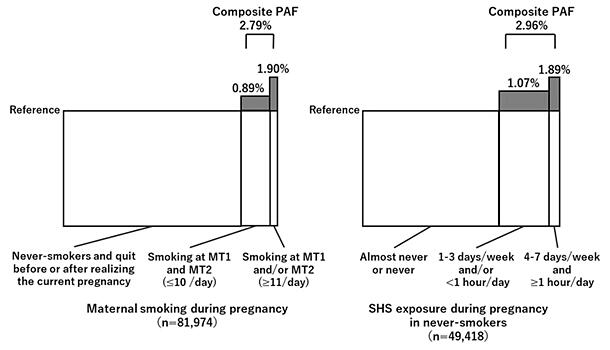
In this study, the research group analyzed data collected from approximately 82,000 pregnant women as part of the "Japan Environment and Children's Study (JECS)" to examine the association between active and passive smoking and placental abruption. In terms of active smoking during pregnancy, mothers were divided into five groups ("never-smokers," "previously smoked but quit before realizing the current pregnancy," "previously smoked but quit after realizing the current pregnancy," "smoking during the first and second/third trimesters: ≤10 cigarettes per day," "smoking during the first and/or second/third trimesters: ≥11 cigarettes per day"). In terms of passive smoking during pregnancy, mothers were divided into three groups ("almost never or never," "1-3 days per week and/or <1 hour per day", and "4-7 days per week and ≥1 hour per day"). Risk ratios and population-attributable fractions (PAFs) were determined through statistical analysis to measure the association of active smoking statuses in the five groups and passive smoking statuses in the three groups with placental abruption.
The results showed that in terms of active smoking, the risk for placental abruption in the "smoking during the first and/or second/third trimesters: ≥11 cigarettes per day" group with the highest cigarette exposure was approximately 2.2 times higher than that in the "never-smokers" group. In terms of passive smoking, the risk for placental abruption in the "4-7 days per week and ≥1 hour per day" group with the highest secondhand smoke exposure was about 2.3 times higher than that in the "almost never or never" group. The risk for placental abruption did not differ significantly in any other active or passive smoking-based groups.
PAF is a measure of the extent to which placental abruption would be reduced if there were no active or passive smoking during pregnancy. PAFs of active and passive smoking were about 2.8% and about 3%, respectively. This was the first study to show that even secondhand smoke exposure increases the risk of placental abruption. Although this was an epidemiological study and, therefore, does not show a direct cause-and-effect relationship, it provides data to support awareness building.
Karumai said, "I believe that various efforts to encourage smoking cessation during pregnancy have been already made, including those through prenatal checkups and maternal and child health programs. In addition to measures against active smoking during pregnancy, efforts to prevent secondhand smoke exposure will be important. Furthermore, policies and educational activities are needed to reduce maternal smoking during pregnancy and secondhand smoke exposure in public places and at home. Moreover, it is often difficult to tell who is pregnant in society. Care must be taken to ensure that no one is exposed to secondhand smoke against their will."
Journal Information
Publication: BMJ Open
Title: Impact of maternal smoking and secondhand smoke exposure during singleton pregnancy on placental abruption: analysis of a prospective cohort study (the Japan Environment and Children's Study)
DOI: 10.1136/bmjopen-2024-089499
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




