A group led by Professor Koichi Ikuta and Program-Specific Senior Lecturer Shizue Tani-ichi (at the time of research) of Kyoto University's Graduate School of Medicine has announced that the IL-7 receptor (IL-7R) is necessary for the survival of regulatory T cells (Tregs) in visceral fat, and that IL-7 produced in visceral fat is important for suppressing type 2 diabetes. This discovery could lead to the development of new therapeutics for type 2 diabetes and the findings were published in the international academic journal The Journal of Immunology on March 19.
Provided by Kyoto University
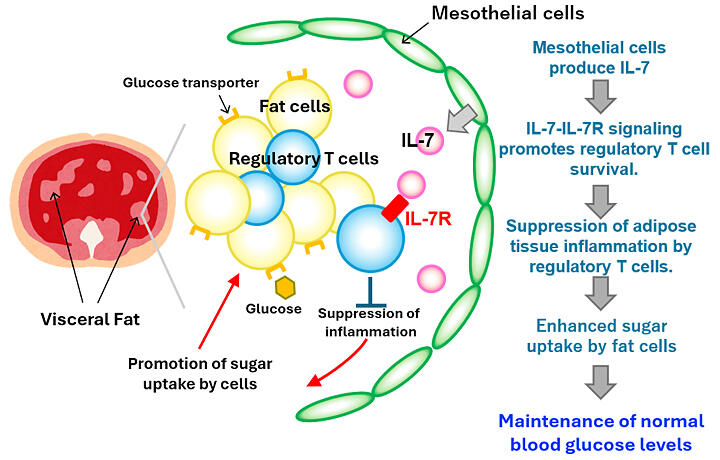
Regulatory T cells (Tregs) suppress autoimmune diseases by inhibiting excessive immune responses. While other T cells express high levels of the cytokine IL-7 receptor (IL-7R) and survive in peripheral tissues in an IL-7-dependent manner. Tregs in lymphoid tissues differ from other T cells by having low IL-7R expression and can survive without IL-7. Although Tregs in visceral fat are thought to play an important role in suppressing type 2 diabetes, the influence of IL-7 on Tregs in non-lymphoid tissues, including visceral fat, remained unclear. In this study, the researchers created mice with Treg-specific IL-7R deficiency and analyzed Treg cell numbers in various tissues.
The results showed that only Tregs in visceral fat were reduced to less than half in IL-7R-deficient mice compared with wild-type mice. There was no difference in Treg cell numbers in the thymus, lymphoid tissues, intestines, or lungs compared to wild-type mice.
The researchers also found that Tregs in the visceral fat of IL-7R-deficient mice had decreased expression of the anti-apoptotic protein Bcl-2. Furthermore, IL-7R-deficient mice exhibited hyperglycemia compared to wild-type mice and developed type 2 diabetes with insulin resistance.
In addition to IL-7, IL-7R also binds to TSLP, a cytokine relatively highly produced in lung and skin epithelium that binds to a dimer of IL-7R and a TSLP receptor. The researchers created TSLP-deficient mice and evaluated the effects on Tregs in visceral fat and blood glucose levels.
In TSLP-deficient mice, Treg cell numbers in visceral fat were slightly decreased, to a lesser extent than in IL-7R-deficient mice, but they still showed hyperglycemia. Detailed analysis of immune cells in visceral fat revealed a significant decrease in eosinophils. Gene expression analysis showed that IL-7 is mainly produced by mesothelial cells, while TSLP is primarily produced by adipose-derived stem cells and macrophages.
Ikuta stated, "This research has revealed that the cytokine IL-7 maintains regulatory T cells in visceral fat and helps maintain normal blood glucose levels. In the future, we expect this to contribute to the development of new therapeutics for type 2 diabetes targeting IL-7 and regulatory T cells."
Journal Information
Publication: The Journal of Immunology
Title: IL-7Rα signaling in regulatory T cells of adipose tissue is essential for systemic glucose homeostasis
DOI: 10.1093/jimmun/vkae064
This article has been translated by JST with permission from The Science News Ltd. (https://sci-news.co.jp/). Unauthorized reproduction of the article and photographs is prohibited.




