A research group from Kyoto University and other institutions announced that they successfully suppressed kidney function decline by transplanting kidney precursor cells derived from human-induced pluripotent stem cells (iPS cells) into mice with chronic kidney disease (CKD). It is estimated that approximately 20 million people in Japan suffer from CKD, and when the condition progresses to end-stage renal failure, patients require dialysis or kidney transplantation. The research group aims to begin clinical trials within several years after confirming safety.
The research group led by Professor Kenji Osafune and Program-Specific Senior Lecturer Toshikazu Araoka from Kyoto University's Center for iPS Cell Research and Application (CiRA) has previously transplanted iPS cell-derived renal precursor cells (nephron precursor cells) into mice simulating acute kidney injury and confirmed their therapeutic effects. The group continued researching toward CKD treatment and successfully created a CKD model mouse that gradually develops fibrosis indicating kidney function decline over 1-6 months.
Provided by Kyoto University Center for iPS Cell Research and Application
However, to use kidney precursor cells derived from iPS cells for human treatment, they needed to efficiently increase these cells, requiring approximately 1 billion cells per person. Thus, mass production of high-quality renal precursor cells with potential therapeutic effects was a challenge.
The research group developed a new method of generating cell aggregates by placing cell clumps of approximately 20,000 cells in each of nearly 100 plate holes, adding a special culture medium (CFY culture medium). This method allows cell expansion to over 100 times the original number while maintaining high cell quality.
Based on these results, Osafune and his colleagues transplanted a large number of renal precursor cells beneath the kidney capsule of CKD model mice. Three days after transplantation, they found suppression in the rise of blood urea nitrogen (BUN) and serum creatinine values, which indicate kidney function decline when elevated. They also observed that fibrosis progression had been halted.
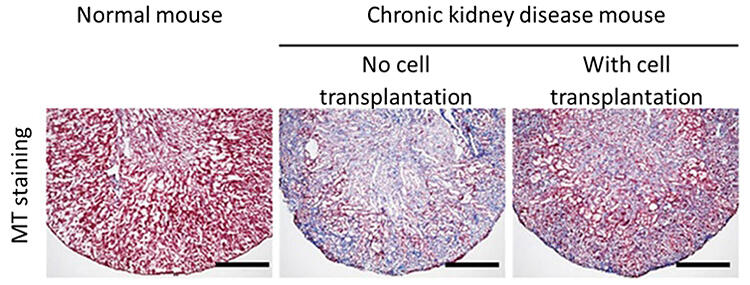
Provided by Kyoto University Center for iPS Cell Research and Application
The research group believes that proteins (VEGF-A) secreted by transplanted cells promoted angiogenesis, thereby mitigating kidney damage.
According to the research group, CKD involves chronic kidney function decline that is difficult to completely cure. As it progresses, it can lead to end-stage renal failure where survival becomes difficult without dialysis or kidney transplantation. Therefore, regenerative medicine using iPS cells offers hope. The research paper was published in the international scientific journal Science Translational Medicine on April 2.
Regenerative medicine using iPS cells is currently the subject of research for practical application in various medical fields. Shinya Yamanaka, Director Emeritus and Professor at Kyoto University's CiRA, developed human iPS cell generation technology in 2007, bringing significant attention to the field. A key feature is their ability to transform into various cell types, with the primary aim being the regeneration of tissue and organs damaged by disease or injury.
RIKEN et al. were the first to perform transplantation for age-related macular degeneration in 2014. Since then, CiRA, the University of Osaka, Keio University, and other institutions in Japan have been conducting clinical trials and applied research for treating various conditions including Parkinson's disease, heart failure, and spinal cord injuries.
On April 17, the CiRA announced clinical trial results of transplanting iPS-derived nerve cells (iPS-derived dopamine neural precursor cells) into the brains of Parkinson's disease patients. They reported motor function improvements in 4 out of 6 patients, suggesting promising effects.
Original article was provided by the Science Portal and has been translated by Science Japan.