From "Talking to researchers - The novel coronavirus (Covid-19) from an immunology perspective and a virology perspective," a symposium held on November 21, 2020 at Science Agora 2020.
To begin with I will explain what sort of reaction the novel coronavirus triggers in our bodies, and in particular the immune reaction.
The single most notable characteristic of this illness is that even when people are infected, because there are not many symptoms it may go unnoticed. Consequently, people end up passing it on without knowing it. In around 90% of people the illness only produces mild symptoms, but approximately 10% become severely ill and around 1-3% die. If the number of patients increases sharply it risks triggering a phenomenon referred to as a medical care collapse--hospital beds fill up and it becomes impossible to treat both people who are seriously ill and people who have common illnesses. The coronavirus infects both children and adults, but the older the patients are the sicker they tend to become, so when community outbreaks occur at facilities for senior citizens, a large number of residents end up dying.
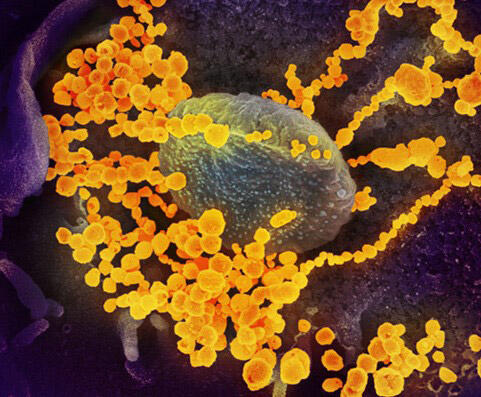
This novel coronavirus is extremely small, having a diameter of just 0.1 micrometers. RNA, the virus' genetic material, is contained inside the virus particle as if it is folded up. The surface of the virus is covered with structures that resemble nails. These are known as spike proteins or S proteins, and one virus particle has around 100 of these spike proteins protruding from it. These spike proteins bind with proteins known as ACE2s, which are found on the surface of human cells.
Large quantities of these ACE2s exist on the epithelial cells of human lungs. While there are individual differences, ACE2s are also present in the mouth, and on the mucous membrane and epithelial cells of the nose, and they are also present on the cells covering the inside of blood vessels and on fat cells. We know that because this virus clings to the epithelial cells of the lungs in most cases, it mainly causes pneumonia. It only takes around 10 minutes for the virus to enter cells, and it takes around 10 hours for it to proliferate within cells. When a single virus particle enters a cell, it proliferates into around 1,000 particles, so if 1,000 cells become infected it means that 10 hours later one million virus particles (1,000 x 1,000) will emerge.
Our bodies are protected through a two-tier structure of natural immunity and acquired immunity
Our bodies are equipped with a defense system that has a two-tier structure--namely, natural immunity and acquired immunity. When a pathogen attempts to penetrate the body from the outside, it faces at least three major barriers. The first two barriers are known as natural immunity. To begin with bactericidal substances that exist on our skin and mucous membranes try to prevent pathogens from entering the body. This is known as the physical and chemical barrier.
However, if there are gaps in that barrier a virus will penetrate the layer inside it. There, phagocytes, which are a type of white blood cell, are waiting for the pathogen, and they either eat it or use a bactericidal substance to kill it. This is natural immunity. It responds quickly, but has no immunological memory. If the body cannot be defended from the virus with this natural immunity alone, the virus will penetrate further. If that happens, B cells and T cells--two types of lymphocyte, a type of white blood cell--take charge by forming antibodies in response to the pathogen that has broken through the body's natural immunity. Those antibodies expel the virus. This is acquired immunity.
Even though natural immunity responds quickly, it does not remember the pathogens it has come into contact with. Acquired immunity is slow to respond, but it remembers the pathogens it has come into contact with, and so if the same virus enters the body again, the body's acquired immunity works powerfully to expel it. Natural immunity is a mechanism that everyone has from the time they are born, and acquired immunity is a mechanism that develops after we are born. Because we have these two mechanisms, even when we come into contact with viruses, we are not readily infected. In all likelihood, even if we were assailed by 100 or 200 virus particles, we could utilize these immunity mechanisms to repel them.
I would like to talk about the vaccines. The vaccination inoculation mimics the viral infection. When that happens, initially natural immunity is stimulated. Once it is activated, acquired immunity next comes into play. It always occurs in this order. When natural immunity is activated, phagocytes kill the virus. When acquired immunity is activated at least three types of lymphocyte go to work. The most important are the "helper T cells." These cells are the "control tower" of acquired immunity, and they kill the virus by issuing B cells with a directive to create antibodies against the virus, for example. Or, the helper T cells will issue its own "brothers," the killer T cells, with a directive and the killer T cells will kill cells that are infected with the coronavirus. When these four cells work in order the virus will be completely expelled from the body.
It is possible that the virus can be killed using natural immunity--the first tier of the two-tier structure--alone. However, in a case where infection has not been prevented with natural immunity alone, it becomes acquired immunity's turn to act. The reason that we know this much is because even people who are congenitally unable to produce antibodies are recovering from this illness. That means that while antibodies are important, we are not expelling the virus with antibodies alone. All the mechanisms of immunity function to expel it. In considering acquired immunity, I believe that the two types of T cells may be more important than antibodies. What is important is the body's resistance strength and immune strength, in other words, a combination of both natural immunity and acquired immunity.
Although we talk about antibodies as one thing, there are actually three types - good ones, bad ones and ones that have no role
Next, I will explain antibodies. Everyone seems to believe that if they are vaccinated, they will form antibodies, and if they have antibodies, they will not catch this illness, but there are in fact three types of antibodies--good ones, bad ones and ones that have no role. To begin with, the good antibodies are antibodies that kill viruses and stop viruses from working. In medical terminology, these are known as neutralizing antibodies. On the other hand, the bad ones are antibodies that end up promoting the viral infection and exacerbating the illness. The role-less antibodies are antibodies that do not possess either function. The term antibodies refers to the three types--good ones, bad ones and ones that have no role--collectively.
In the case of infections by many viruses--and influenza is one such example--it is primarily the good antibodies that are activated and so the illness improves. In the case of AIDS, however, although a large number of antibodies are produced following infection, most of them are role-less antibodies and so cannot kill the virus. Cats also become infected with coronaviruses but when a virus vaccine was made and administered to cats, they conversely became sicker. When this was studied it was discovered that although a large number of antibodies were being produced, many were bad antibodies. So, there is no guarantee that good antibodies alone will be produced.
The issue of how many antibodies are being produced and whether it is a lot or a little is often raised, but simply measuring the quantity of antibodies is in itself not very meaningful. The quantity of good antibodies that have been produced has to be accurately measured, but regrettably the measurement of good antibodies cannot be carried out by private-sector institutions. It can only be performed by laboratories with sophisticated equipment.
We know that when people become infected with the novel coronavirus, the milder a person's symptoms are the fewer the antibodies that are produced, and the more serious a person's illness is the greater the volume of antibodies produced. If the antibodies that are produced are good antibodies, then people should not be becoming seriously ill. Technically, patients with a large number of antibodies present should only be experiencing mild symptoms, yet the opposite situation is occurring.
On the other hand, when people who have recovered from the novel coronavirus are examined there is no question that they have produced good antibodies. I said that people who become seriously ill have a large volume of antibodies, but it seems likely that what is being produced are large numbers of antibodies other than good antibodies--namely, role-less antibodies or bad antibodies. Conceivably, the reason they become seriously ill is because this balance has gone awry. What we would like to know is what produces the good, role-less and bad antibodies, respectively. There appears to be extremely large individual differences, but regrettably, it is not yet known what type of person will produce what type of antibodies, and in what ratios.
Earlier, I mentioned that for immunity to operate, T cells are also important, not just B cells, and recently we have come to understand something regarding what T cells do in relation to this novel coronavirus. This same insight has been gained in seven countries worldwide. Namely, in 20-30% of people not infected with the virus, there are T cells that are able to respond to it. This is a surprise to immunologists. Generally speaking, in an individual who has not been infected with a particular viral illness, the T cells that respond to the virus causing that illness will be virtually undetectable. However, in the case of the novel coronavirus, 20-30% of normal individuals who have not been infected will already possess T cells for the virus.
What we know at present is that these T cells that are responsive to the coronavirus appear to have been produced in response to other types of coronaviruses. This kind of immunity is known as cross-immunity. We say that if you have been infected with Virus A then you will have cross-immunity to Virus B. It appears that this is the situation being seen here. Currently four types of coronavirus are known to cause influenza, and it is conceivable that individuals who have had those viruses will have cross-immunity to the novel coronavirus.
We will need to live with the novel coronavirus for several years - preserving your lifestyle rhythm is important
Anyone hearing this could well conclude that if they have been infected with a coronavirus of some sort, they will be unable to catch the novel coronavirus. Regrettably, however, this is an area that is still not properly understood. Lymphocytes are cells comprising a countless number of clones, and one cell possesses receptors for one type of antigen. For example, if a certain coronavirus joins with a cell, this clone alone will steadily increase. In some cases, even individuals who have not had the novel coronavirus have cells such as this.
However, the issue is whether these cells are beneficial or harmful to our bodies. In other words, are individuals who possess antibodies that are responsive to coronaviruses unlikely to catch the novel coronavirus, or are they conversely likely to catch it? Regrettably, we do not know the answer to this question.
One reason we do not know is because the incidence rate of novel coronavirus infections is low. Even in countries where infection is severe, only a few people in every 1,000 become infected. Research such as this has so far only been carried out on sample groups numbering in the hundreds, and in units of 100 people, coronavirus infection does not appear. Without studying a sample size somewhere in the vicinity of tens of thousands of people or hundreds of thousands of people, in countries where infection is really severe, we will be unable to determine whether individuals who possess these coronavirus-responsive T cells are unlikely to catch the coronavirus but likely to fall seriously ill if they do, or more likely to catch the coronavirus and likely to fall seriously ill if they do.
It seems plausible that a certain percentage of us possess some immunity to the coronavirus, but we do not know whether that works in a good way or a bad way. Accordingly, I believe we have to keep company with this virus while exercising deep caution. It is conceivable that achieving herd immunity against this novel coronavirus will not be simple. That being the case, we will likely have to live with this virus for several years.
So, what should we do? On top of doing the essential and fundamental things to avoid the coronavirus--and doing them properly--it will be important to maintain your body's immune strength. The key to achieving that is to not disrupt the rhythm of your lifestyle. When your body's internal clock is functioning well, you have an appetite, you sleep well at night, and it simultaneously becomes possible to maintain your immune strength also. Another very important point is to exercise. When you move your body, you use your bones and muscles. The fact is that many of the immune-regulating substances that are important for maintaining this immune strength are produced in your muscles and bones. Furthermore, we know that large amounts of them are produced when you exercise.
One final point is to secure accurate knowledge of the coronavirus. By that I mean "be fearful, not terrified." Adopting practices that are based on logic is the most important way of tackling this virus. When you can do that, then you can issue yourself with "alerts," which will lead you to take personal responsibility for own body, I believe. For the time being we will live with the virus by making appropriate efforts ourselves. I think this point is the most important of all.
Masayuki Miyasaka, M.D., Ph.D.
Professor Emeritus of immunology at Osaka University;
Born in Ueda City, Nagano. Graduated from Kyoto University Faculty of Medicine. Obtained his PhD at the John Curtin School of Medical Research, Australian National University. After undertaking research activities at the Basel Institute for Immunology, Switzerland, he was made head of the immunity research department at the Tokyo Metropolitan Institute of Medical Science. In 1994, he was appointed as a professor at the Biomedical Education and Research Center, Osaka University Medical School, and in 1999, he was made a professor at the Graduate School of Medicine, Osaka University. He is currently Specially Appointed Professor at the Immunology Frontier Research Center, Osaka University, and Professor Emeritus at Osaka University.
Original article was provided by the Science Portal and has been translated by Science Japan.