The National Cancer Center Research Institute has announced on February 29 that they have clarified the landscape of genetic mutations in Japanese cancer patients, which differ from those in patients in the United States, European countries, and other regions. Genetic mutations were analyzed using the "cancer gene panel test" data of approximately 50,000 patients. The average percentage of patients with mutations that can be targeted by cancer drugs was about 15%. The study provided valuable data for "cancer genomic medicine," in which genetic mutations and the like are clarified and in turn drugs likely to be effective are selected. The National Cancer Center Research Institute intends to continue the analysis of the data to improve treatment outcomes.

Provided by the National Cancer Center
Genomic medicine: Finding the right treatment for each patient
The human body has about 37 trillion cells. The nucleus in each cell contains chromosomes carrying genes. The genome is the whole of the genes and genetic information contained in the chromosomes. There are 20,000 to 30,000 different genes in the genome of a person, and each gene has a different "command function" to create the body.
The genome of a person consists of sequences of 6.2 billion bases inherited from their parents, and the differences in the sequences of certain bases determine each person's characteristics. These characteristics include appearance and personality, as well as susceptibility to disease, reactions to medication, and adverse reactions.
Genomic medicine utilizes these differences for medical care purposes, and such information is used in cancer treatment. A decisive factor in the effectiveness of cancer genomic medicine is the cancer gene panel testing. The "next-generation sequencer," which reads a large amount of genomic information at high speed from tissue taken via biopsy, intraoperative sampling, and other means, can examine tens to hundreds of genes simultaneously. Cancer gene panel testing has rapidly become popular since insurance coverage began in 2019. Once the genetic mutations or alterations are determined and the characteristics of the patient's cancer are known, doctors can determine the appropriate treatment for the patient. From the patients' point of view, gene panel testing is a tool to find "drugs that target changes in the targets own genes" or "molecular targeted drugs."
It is important to note that genes do not directly create cancer tissue. Cancer is a disease occurring when genes fail to function properly for several reasons. Except for a minor form of cancer known as "familial tumors," in which genetic mutations are inherited, most cancer cells occur as a result of acquired genetic mutations in certain somatic cells due to lifestyle, smoking, aging, or other factors. These cancer cell-specific genetic mutations are not inherited by the next generation.
Currently, this test is conducted at specific types of hospitals such as "designated core hospitals for cancer genomic medicine," "designated hospitals for cancer genomic medicine," and "cooperative hospitals for cancer genomic medicine." The test results are collected at the "Center for Cancer Genomics and Advanced Therapeutics" at the National Cancer Center with the consent of the patients. The data collected are limited to those from patients with cancers that did not respond adequately to standard treatment, rare cancers for which there is no standard treatment, and cancers of unknown primary. However, as genetic mutations unrelated to cancer may be found in the tests, it is important that hospitals capable of providing adequate explanations and consultation regarding genetics are available.

Provided by National Cancer Center and translated by Science Japan

Provided by the Center for Cancer Genomics and Advanced Therapeutics, National Cancer Center
Big differences among different types of cancer
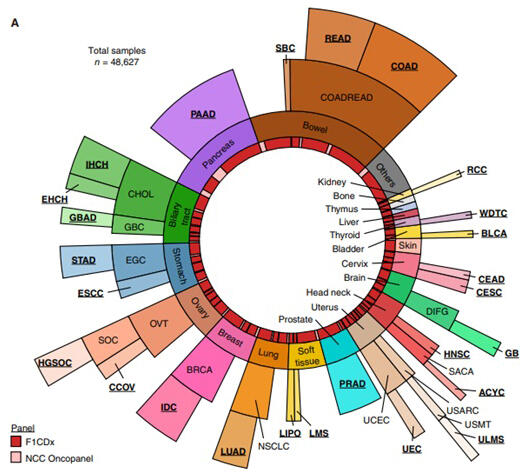
According to the National Cancer Center Research Institute, the research team analyzed 48,627 cases collected at the Center for Cancer Genomics and Advanced Therapeutics between June 2019 and August 2023. The most common sites of cancer included the colon/rectum, pancreas, and biliary tract.
The analysis showed that genetic mutations targeted by therapeutics were found in 15.3% of the cases collected. Among the 26 cancer types, thyroid cancer was the highest at 85.3%, followed by breast cancer at 60.1% and lung adenocarcinoma at 50.3%. Thyroid cancer was the highest likely because diverse drugs have been developed. Meanwhile, percentages of mutations in cases of salivary gland cancer, liposarcoma, and renal cell carcinoma were lower than 0.5%, suggesting that therapeutic agents are difficult to find for these types of cancer. It was also clear that there are significant differences among the different types of cancer.
According to the National Cancer Center Research Institute, there have been studies analyzing the data from Europe and the United States, but this is the first study analyzing the data from Japanese patients. In this study, biliary tract cancer, stomach cancer, and cervical cancer, which are common among Japanese, were also included in the analysis. In comparison with data from Caucasian patients in the United States, the proportion of cases in which a genetic mutation or other target of a therapeutic drug was found was about two-thirds.
The research team led by Dr. Keisuke Kataoka, Chief of the Division of Molecular Oncology at the National Cancer Center Research Institute (concurrently a Professor at the Department of Internal Medicine at Keio University School of Medicine) attributes these results to the fact that many cases of intractable cancer for which effective therapeutic drugs are scarce, such as pancreatic cancer and biliary tract cancer, were included in the analysis.

Provided by the National Cancer Center
Provided by the National Cancer Center
Urgent need to promote therapeutic drug development
In December 2019, the Ministry of Health, Labor, and Welfare (MHLW) has reported that only about 10% of cancer patients were able to reach appropriate therapeutic drugs. The MHLW analyzed 805 patients who had undergone gene panel testing at 134 hospitals by the end of October of 2019, and showed that the drugs were found in 88 (10.9%) patients.
This result is close to that found in the current analysis conducted by the National Cancer Center Research Institute, that is, "genetic mutations targeted by therapeutics were found in 15.3% of the cases collected." The details of the cancer types included in the MHLW survey are not known; nevertheless, the results highlighted a major issue in current cancer care: the difficulty in finding appropriate and effective medication for cancer. Kataoka, division chief of the Research Institute, also pointed out the urgent need to accelerate the development of therapeutic drugs for intractable cancers and other types of cancer that are common among Japanese people, based on the characteristics of cancer genomic abnormalities in the Japanese patients.
In addition to analysis of gene panel test data, the National Cancer Center has conducted genetic analysis of patients with various types of cancer and published many interesting research findings. For example, in March 2023, the National Cancer Center has announced that alcohol consumption by people constitutionally unable to metabolize alcohol efficiently increases the risk of developing difficult-to-treat "diffuse gastric cancer," such as "scirrhous gastric cancer." This is a finding of genetic analysis of cancer tissue from more than 1,000 patients and expected to contribute to the prevention of disease onset and the discovery of treatments.
In January 2023, the National Cancer Center has also announced a method of analyzing the cancer genes using blood samples collected from patients who have undergone surgery for colorectal cancer to evaluate the risk of recurrence. The effectiveness of treatment with anticancer drugs is believed to vary from patient to patient. Therefore, the recurrence risk evaluation for each patient is useful in making decisions about appropriate anticancer drug treatment after surgery. This is an achievement that will contribute to appropriate treatment with anticancer drugs, to which adverse reactions are not unusual.
Must not lead to genetic discrimination
Various studies examining patients' genes support advances in cancer treatment. Factors underlying the research advancement include an improved understanding of genetic mutations associated with each type of cancer. However, genetic information, which differs from individual to individual, is the "ultimate form of privacy." Its protection and prevention of discrimination is a prerequisite for advancing cancer genomic medicine. There should be no inappropriate handling of genetic information in situations such as insurance policy purchase or employment.
The "Genome Medicine Promotion Act" for the promotion of genomic medicine in an appropriate, fair, and equitable manner was enacted in the 211th ordinary Diet session in June 2023. Although the new law clearly states, among other things, that no unfair discrimination should be made based on genetic information, the new law lays out principles and is "general" in nature. Thus, specific measures are required to establish research and healthcare systems that meet the principles of the new law.
Regarding cancer and other diseases, individual patients with the same disease have different mutations in genes related to the cause of the disease. Knowing which part of the gene is responsible for the disease may open the path to find a patient-specific treatment that is effective in terms of physical burden, cost, and use of expensive drug. Expectations are high for genomic medicine. Therefore, the promotion of genomic medicine and the genetic information protection/discrimination prevention are like the two wheels of a cart.

Provided by the Ministry of Health, Labour and Welfare and translated by Science Japan
(UCHIJO Yoshitaka: Science Journalist)
Original article was provided by the Science Portal and has been translated by Science Japan.