-

- Writer
- Maho Ise
-

- Interviewer
- Yūya Nishimura
-

- Editor
- Eriko Masamura
During his high school days, Prof. Hideki Katagiri knew that the path he would follow was one that "was involved in human lives," and "of service to society." Today, while serving as a physician treating patients in a clinical environment, he is also continuing his academic research into diabetes and obesity, two diseases which afflict a wide number of people in modern society.
So, how did Katagiri develop into a researcher who strives to "shed light on every mechanism of living things?" It is here that the impact of advice from several mentors can be felt.

Tohoku University Graduate School of Medicine
"'Research is romance.' However, I want to conduct research that helps people"

Please tell us about your interests when you were a junior and senior high-school student.

I was born and raised in Osaka, but I attended junior and senior high school in Kobe City. My junior high was stimulating, and I had a lot of freedom, so I enjoyed my time there. But at the end of my second year of high school, the timing where students in Japan had to decide between continuing with the sciences or humanities, I had an extremely hard time making a decision. At the end of the day, I decided to pursue a future in medicine and life science, with the mindset that "nothing is more important than being involved with human life."
Nishimura: If you had such a hard time deciding, then you must have had at least considered following a path in the humanities, right?
Katagiri: That's right, I did. I considered the option of "serving society" by becoming a public servant or something similar.
Nishimura: When I was a high school student, I didn't think about life, or how I could be of service to society at all, so I think that your mindset is pretty amazing. Do you still continue to have the drive to do so even now?
Katagiri: I don't think that I am special or anything, so it was probably a result of the school culture. Many of my classmates have also excelled in a wide range of fields. I just felt that human life was the most important thing and continue to do so today.
Nishimura: After carefully considering your options, you went on to study at the faculty of medicine at the University of Tokyo, right?
Katagiri: I did get into medical school, but I thought that I wanted to become a medical researcher more than a doctor, and so thought of pursuing a career as a researcher. In those days, university medical schools followed a curriculum that covered general education in the first and second years, basic medicine in the third and fourth years, and clinical medicine in the fifth and sixth years. When I was a fourth year, I deeply admired Professor Tomio Tada (*1), a professor of immunology, and for a brief period was allowed to attend his laboratory. When I look back now, I was very fortunate to experience that environment, where he didn't just take us on lab trips, but also provided a wide range of life experiences such as when he treated me to a whole roasted sparrow (a delicacy in Kyoto).
Katagiri: Around that time, one day I went to the basement cafeteria of the faculty of medicine to have lunch with the professor. We often went to lunch together, but on that day, he asked me, "What exactly is it that you want to do?" I had a number of allergies during my childhood, although they weren't serious, and so I answered, "I'd like to undertake research to cure immune-related diseases such as allergies." No matter how you think about it, I don't think my answer was strange at all, but the second Professor Tada heard it the color drained from his face, and he replied, "We really aren't on the same wavelength, I think you should get out of my lab." This came totally out of left field, and I was in shock that I had suddenly been excommunicated. All I could do was dejectedly ask myself, "Did I say something wrong?"
When I thought about it later, I took Professor Tada's thought process as "Research should be romantic," suggesting that it shouldn't be done with a calculating end goal like "curing a disease." However, I never visited his laboratory after that and never saw him again. Then, time passed, and I attended Professor Tada's memorial service after he passed away. Many of the visitors stated, sort of, "I was excommunicated ten times" in their address, which made me realize that "excommunication" was a usually used expression that he liked. I took his words to heart and distanced myself from him, but I still found the idea of "research is romance" incredibly appealing. Even now, I continue to do research with this mindset, grateful that I had the chance to meet him.
However, the feeling of "wanting to be of service" is inherently present in me, so I consider it a blessing to be able to experience both feelings of "romance" and "being of use to others."
- *1Tomio Tada: Immunologist and writer. He led the Immunology laboratory at the University of Tokyo.
The words "Departments of internal medicine are places for research" motivated me to have two careers: As both a researcher and physician
Nishimura: How did you proceed in your fifth and sixth years after that?
Katagiri: Right after that, clinical lectures began. At that time, I considered clinical practice as an opportunity to receive training to efficiently learn special skills, such as being able to make quick judgments and respond to patients. Due to this, I felt as though I was transitioning from academic study to vocational education, almost as if I were moving from a university to a vocational school. That is why I wanted to decide on my future field of research before finishing my fourth year.
Because of this I thought that I would just listen to the lectures with one ear, but then I had a fateful encounter. It was a lecture by Professor Nakaaki Ohsawa (*2), who at the time was an Associate Professor at the Third Department of Internal Medicine of the Faculty of Medicine at the University of Tokyo and specialized in endocrinology. I don't really remember the actual content of the lecture, but I think it was something about recently discovered nuclear receptors for steroid hormones rather than about a hormonal disorder such as Cushing's syndrome (*3).
I had thought until then that hormone receptors were only located on the surface of cell membranes and remember how impressed I was by the new concept in the field of life science, and how the research was progressing. The lecture that day was held in a classroom where we sat in tiered seating, and as soon as the class was over, I rushed down the stairs to approach the professor. That's how excited I was. When I asked him, "Is it possible to do this kind of research in internal medicine too?" he replied, "What are you talking about? Departments of internal medicine are places for research." These words from Professor Osawa changed my life.

Your memory is so vivid.
Katagiri: It was such an important moment. Until then, I felt pressured to decide on a specialty by the end of my fourth year. However, after that, I realized that studying internal medicine would also be a good option. Osawa's words made me decide to study to become a physician and do my residency.
Nishimura: Connecting back to what you said earlier about being a "medical researcher rather than a physician," would you have been interested in being a physician if it meant being an internist who was practicing as a physician while learning?
Katagiri: Yes. I aim to do academic research rather than to simply learn. My path became clear when I realized that there was an environment in which I could be a physician while pursuing academic research. In the end, I was able to follow a path that, to a certain extent, satisfied my desire to "be involved in human lives," and "be of service to society" while serving as both a researcher and a physician.
Nishimura: You have always been dedicated to two tasks: being a physician in a clinical setting and pursuing academic studies as a researcher.
Katagiri: For the first two years after I became a physician, I was only an intern and focused solely on medical training without conducting any research. However, I have simultaneously practiced medicine and conducted academic studies since my third year.
- *2Nakaaki Ohsawa: Professor Emeritus at Osaka Medical College. Former chairman of the Aino Institute for Aging Research.
- *3Cushing's syndrome: A collective term for a disease characterized by various symptoms such as truncal obesity, moon face, and diabetes caused by excessive secretion of cortisol, a hormone considered necessary for maintaining life.
Exploring "obesity" and "diabetes" leads to understanding of the mechanisms of all life
Nishimura: I think "obesity" and "diabetes" are keywords in your research themes. Could you share when you came across these themes, and when you decided to make them the focus of your research?
Katagiri: It was when I met my most influential mentor, Professor Yoshitomo Oka (*4). I was a member of the tennis club during my university years. Oka was an alumnus of the club and an excellent player who even made the top eight in the intercollegiate game (All-Japan University Championships).
The tennis club held an alumni match twice a year, and it was at one of these that I met Oka and spoke to him about my career path. I had a strong interest in immunology, so I constantly asked him for advice on which laboratory I should go on to among laboratories focusing on clinical immunology. One day, while talking about his own research, Oka said, "You know, we just want to understand how we are living." This "we" carries two meanings, "we as researchers" and "we who are alive," and his message of, "I want to understand the mechanisms of how we are living," resonated very deeply with me. Oka's research themes were glucose metabolism and diabetes.
Diabetes is a disease caused by abnormalities in glucose metabolism and affects many people. Glucose metabolism, the process of using and storing ingested sugar, is a fundamental mechanism of life itself. Since a slight deviation in this process leads to diabetes, I thought that my own research into exploring the mechanisms of life could potentially benefit many people. Above all, even if it's vague, I thought having the idea that "this might be helpful to someone" rather than "this is useless" while conducting research could serve as my support. That is why, when I heard Oka's words, I made up my mind and joined his diabetes research laboratory.
Nishimura: After hearing that, I thought that this could change our perspective on diabetes. While it is directly connected to human life and the mechanisms of the human body, it is also a disease. It seems to be a rewarding challenge to work on as both a physician and as a researcher.
Katagiri: You are right, and it was exactly what I was looking for, but I had never considered researching diabetes until I heard Oka's words. That's why I kept talking to him, a diabetes specialist, about "which laboratory would be best if I wanted to work on immunology."
Nishimura: I have read your report on the KAKEN database, and it seems that you were the first principal investigator on the research project "Development of gene therapy for diabetes associated with obesity" from 2003 to 2004.
Provided by Katagiri
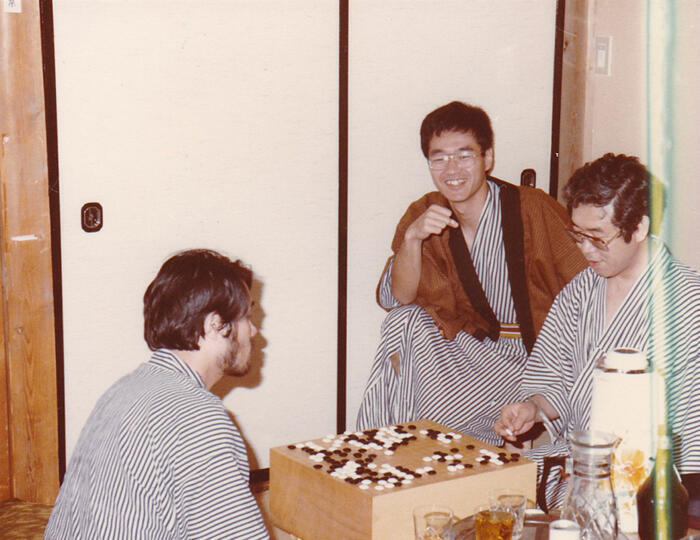
Katagiri: Yes, that is correct. However, I started my research under the guidance of Oka in 1989. When considering human glucose metabolism, many people know that when blood glucose levels rise after eating, insulin, which regulates glucose metabolism, is secreted to aid in glucose transport into cells. For approximately 10 years after the beginning of the research under the guidance of Oka, I worked to shed light on this mechanism—how insulin is secreted in response to an increase in blood glucose and how the secreted insulin lowers blood glucose levels.
At first, I focused on the structure and function of glucose transporters, that Oka was researching.
Nishimura: Could you please explain a bit more about glucose transporters?
Katagiri: Since cells are surrounded by lipids and glucose is water-soluble, glucose is normally repelled by the lipids and is unable to enter the cell. Therefore, glucose transporter membrane proteins bind to glucose and carry it inside, allowing entry into the cell. I had been advancing research into this mechanism, which is shared among organisms ranging from humans to E. coli.
Next, through outpatient care at the hospital, I found patients with a mutation in their glucokinase gene (*5) and mitochondrial DNA (mtDNA) (*6) and began research on the mechanism of insulin secretion when blood glucose levels rise. The β-cells responsible for insulin synthesis and secretion are clustered in island-like cells called "pancreatic islets of Langerhans," which are scattered throughout the pancreas. When the function of these β-cells cannot be adequately maintained, insulin secretion function declines, leading to the onset of diabetes. From an analysis of patients with glucokinase or mtDNA mutations, it was discovered that the mechanism through which β-cells recognize elevated blood glucose levels is also present in humans.
Furthermore, insulin secreted from β-cells acts on fat and muscle cells to move glucose transporters to the cell surface, thereby increasing glucose uptake in these cells and lowering blood glucose levels. I conducted research on which molecules within the cells are involved in this mechanism and how it works, obtaining a degree on this subject.
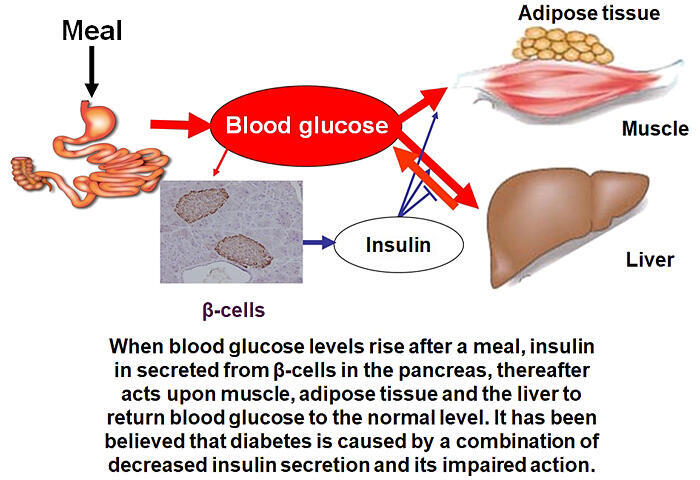
However, these themes eventually became fiercely competitive. I gradually lost the enjoyment from advancing my research. I thought that if there were others who wanted to advance research on the same topic, I might not need to pursue it myself. I even considered stepping back from research for a while. At this time, Oka, who was then at Yamaguchi University, moved to Tohoku University. He approached me and said, "Let's go to Tohoku University together." Until then, I had only been conducting research with one or two people. Oka invited me saying, "You can do research with a team." In 2001, I moved my research and clinical activities to Tohoku University.
Katagiri: The first thing I worked on after moving to Tohoku University was research on how to introduce genes that burn fat in mice in order to improve obesity and diabetes. All the new members I met in the new environment were physicians, and to unite our minds and advance our research goals, I thought it would be more motivating for all of us to focus on something that could improve the condition or lead to potential treatments, rather than creating a model that would worsen the condition. I thought that if we could create a condition in which energy expenditure increases in the setting of obesity, it could be suppressed.
To achieve this, we first tried to induce the expression of genes that burn fat in both the liver and adipose tissue. When we increased the energy expenditure in the liver of mice fed a high-fat diet, fat in the liver burned and adipose tissue shrunk even further. This suggests that adipose tissue is aware that fat in the liver is burning and that a mechanism to acceleratedly supply fat to the liver from adipose tissue exists. In addition, when energy expenditure increased in some adipose tissues, the pathological phenomena that occur in other tissues during obesity were nullified. With this trial, I thought it was extremely interesting to observe how various bits of information are exchanged within the body, signaling messages such as "there is not enough energy here" or "there is too much energy here," and how these signals coordinate to maintain a balance.
- *4Yoshitomo Oka: Professor Emeritus at Tohoku University. Former Professor at the Division of Molecular Metabolism and Diabetes (Department of Diabetes and Metabolism) at Tohoku University Graduate School of Medicine.
- *5Glucokinase gene mutation: Glucokinase is an enzyme that catalyzes the conversion of glucose to glucose 6-phosphate, the first step in intracellular glycolysis in the liver and pancreas. Mutations in the gene coding glucokinase cause a type of diabetes.
- *6Mitochondrial DNA mutation: Mitochondria contain genetic information different from that in the nucleus. Mutations in these genes may lead to various pathological conditions, such as encephalomyopathy. They are also one of the causes of diabetes due to decreased insulin secretion.
Why does "running with your legs" help you lose belly fat instead of in the legs?
Nishimura: When you introduced this gene that increases energy expenditure, did you anticipate that there was already an exchange of information between organs?
Katagiri: Yes, that's right. For example, many people run to lose weight. When you run, even though it is your muscles that consume energy, fat is burned in your adipose tissue, which leads to weight loss, right? It may seem like a completely obvious concept, but it makes me extremely curious about what's happening between using muscles to run and burning fat to lose weight.
Nishimura: The question is why does running slim down your waistline, right? As the leg muscles are being used, the legs should slim down, but they actually become thicker. Something strange is occurring, but I hadn't ever thought about it before. This is "something that is obvious when it is pointed out." I am surprised that I had never thought about it until you just mentioned it. By the way, are inter-organ networks commonplace, or is this a theme for the future?
Katagiri: The topic of communication between organs itself is not new, as is the case with hormones, for example. However, we are fortunate to have discovered that nerves are the intermediaries for these interactions.
The person who introduced me to the world of the autonomic nervous system was Professor Emeritus Akira Niijima (*7) of Niigata University, who was 40 years older than me. Although he had already retired, he had set up a laboratory in his home and continued his research independently. When I told him about our experimental results, he was excited along with us, and kindly gave us detailed instruction on how to handle the autonomic nervous system. At that moment, I thought to myself, "Science is truly wonderful, transcending age and experience and allowing us to enjoy the excitement together," and "I am really glad I am doing science."
Nishimura: Following this, your research connected to the autonomic nervous network, right? After looking at each of your approaches individually, it seems like you conduct your research systematically. Did you have this strategy in mind from the start, or did it gradually develop as you worked on it? Could you share more about this?
Katagiri: Well, this research on inter-organ networks began with changing the metabolism in one organ and then seeing what happens in other organs. For instance, in physics, if we were to launch a rocket to the moon, we would make precise predictions about the landing point and time and then proceed to executing the launch. However, our approach is different, in that we change the metabolism in one organ and observe the reaction in other organs without preconceptions. However, we tried to make the change in metabolism as one of the phenomena that occur in obesity.
If during obesity, a phenomenon we call 'A' occurs, and we find an event where the occurrence of 'A' in one organ triggers the occurrence of 'B' in other organs, we can then observe "Whether the elimination of A in a state of obesity triggers the disappearance of B."
Nishimura: I see.
Katagiri: I said I had no preconceptions, but there was one thing that I expected. When a person becomes obese, insulin becomes less effective. However, in response to this, the number of β-cells in the pancreas increases, and more insulin is secreted. In other words, when insulin becomes less effective, the human body responds by increasing the number of β-cells to produce more insulin so that insulin is activated to protect the body from elevated blood glucose levels. Therefore, while reproducing each phenomenon that occurs during the obese state as 'A,' I had always wondered whether we would come across the phenomenon of the increase in β-cells in the pancreas as 'B.'
- *7Akira Niijima: Former Professor Emeritus of the Faculty of Medicine at Niigata University.
"The possibility of completely curing diabetes using the body's self-curing mechanism" became apparent during the course of research
Nishimura: I would like to ask a bit more about inter-organ networks. What have you discovered through your research, and how far do you think it can go?
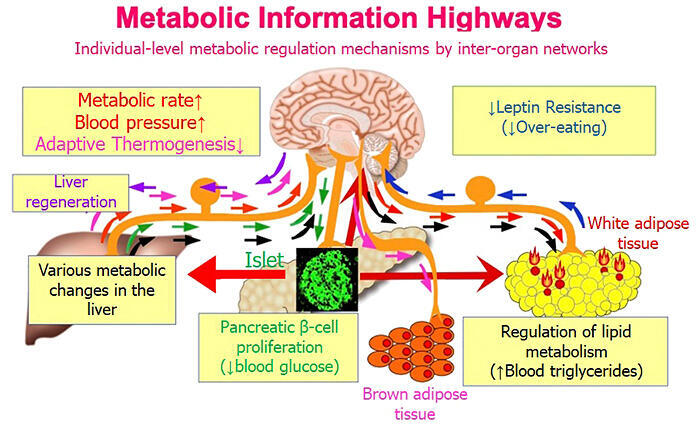
Katagiri: Initially, we conducted research on increasing energy expenditure. However, we discovered a phenomenon where "accumulation of fat in the liver causes fat to be burned in adipose tissue" and published the findings in 2006. We also discovered the importance of the autonomic nervous system, in creating a network that runs from the liver to the brain and then to adipose tissue, as a mechanism for communicating information, that fat has accumulated in the liver, to adipose tissue.
Nerves are basically the link between the brain and the organs. The nerves do not run directly from the liver to the adipose tissue. In other words, the involvement of the autonomic nervous system implies that the brain always serves as a relay point in the inter-organ network between the liver and adipose tissue. Therefore, we were able to propose a new concept in which the brain serves as a conductor, monitoring the metabolic status in the liver, sending pinpoint commands to the adipose tissue, and controlling the metabolism of the whole body so as not to lose harmony.
We then conducted a number of studies that not only looked at instances where "the liver stores fat," but also at where "glucose uptake is increased in the liver," "amino acid uptake is increased in the liver", and "insulin becomes ineffective in the liver." In other words, we conducted several types of research to expand its horizontal reach. In this process, various inter-organ networks were discovered, and it became evident that the autonomic nervous system and brain are involved in all of these mechanisms.
From these findings, we could show that information about various metabolic conditions was exchanged within the body using nerves, and that the brain continuously monitors the metabolic status in all organs of the entire body and sends various signals to each organ to ensure optimal conditions.
To gain acceptance for our discovery that metabolic control is achieved through inter-organ networks, we believed it was necessary to demonstrate that this mechanism is not just occasionally utilized but operates universally in a variety of situations. Therefore, it was a significant achievement for us to show this through horizontally expanded research.
Provided by Katagiri.
Katagiri: However, at the same time, I was given advice that "as the person who discovered this, you should delve deeply into understanding the underlying mechanism, rather than pursuing the horizontally expanded research," which was an opinion I agreed with. Therefore, I decided to focus on specific targets within the multiple inter-organ networks and proceed with research to gain a deeper understanding.
The most intriguing aspect of inter-organ networks for me was the mechanism by which β-cells increase during obesity. I thought that if we could apply this mechanism to humans, we may be able to increase the number of β-cells by utilizing the inter-organ networks inherent in the body, which would allow it to produce sufficient insulin and potentially cure diabetes. In fact, we discovered that when one specific intracellular signaling pathway is activated in the liver, similar to what happens during obesity, the number of β-cells increases dramatically. Therefore, my colleagues and I decided to delve deeper into this system.
First, regarding the mechanism of the increase in the number of β-cells, we clarified the neural network that runs from the liver to the brain and from the brain to the pancreas. Next, we were able to shed light on the mechanism by which metabolic information can be selectively transmitted to the pancreatic islets of Langerhans and the molecular mechanism behind the increase in β-cells in them. Through these processes, we found that the vagus nerve (*8), a component of the autonomic nervous system, is involved in communication from the brain to the pancreatic islets of Langerhans.
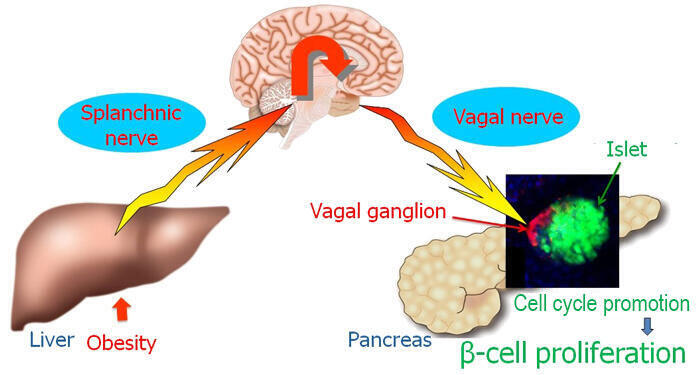
Provided by Katagiri
Katagiri: Then I thought, "I want to find out ways of activating these nerves myself to increase the number of β-cells." I thought that doing so would lead to a treatment method in the future. However, to achieve this, we needed to show whether simply activating the nerve would indeed increase the number of β-cells.
To achieve this, we developed a system for activating only the part of the vagus nerve that innervates the pancreas without activating the parts that innervate other organs. Although we are still in the stage of experiments using mice, we demonstrated that activating these nerves dramatically increases the number of β-cells and enhances insulin secretion. We believe that if we can effectively use this mechanism, it may be possible to increase the number of β-cells in the appropriate locations, i.e. within the pancreas, in the body.
We believe that increasing the number of β-cells in the pancreatic islets of Langerhans using the body's own mechanisms and cells will lead to a "complete cure for diabetes." Alternatively, preventing diabetes by reversing the progression of the prediabetes stage is also possible. We are finally beginning to move in that direction.
Nerves can be activated via electrical or mechanical stimulation. However, as there are numerous patients with diabetes, we are conducting exploratory research with the idea that it may be beneficial if substances contained in medications, supplements, or food could serve as alternatives for easier activation of the nerves.
Ise: From the patient's perspective, oral administration sounds more user-friendly than receiving injections.
Katagiri: That is a good idea because anything that we eat is absorbed in the digestive tract and then goes immediately to the liver. If we can increase the number of β-cells or adjust the number to a desirable level in anticipation of a decrease, it may be possible to reduce the onset of diabetes or even completely cure the disease itself. Because there are several types of diabetes, this may not be applicable to all of them. However, we are conducting research with the aim of curing the types of diabetes that account for a substantial proportion of cases.
Nishimura: Wow, that's impressive, going from narrowing down the target to what you have just told us. I understand that there has been progress in clarifying the mechanism by which stimulation of the vagus nerve activates and increases the number of β-cells. How can this mechanism be reproduced? Is this through medication or other engineering approaches? I think how we do it is still a question for the future. Although it sounds like it is not easy, I don't think it is impossible either. In terms of feasibility, what are your thoughts on whether it is achievable?
Katagiri: I am not sure. If we were to liken it to the moon landing, I believe it is something we will only know for sure once we have actually landed. Because research involves delving into something new, it is often unclear what the correct answer is during the process. I believe we operate in a world where only those who persistently navigate through trial and error, despite uncertainties, eventually reach the point where they can say, "This path was the right one." Right now, whether the ultimate goal is the moon or the much farther away Pluto, my honest opinion is that we will not know unless we try.
Nishimura: I feel as though this project is not just blindly moving forward, but rather, the dream may be something beyond what has been built up so far. I first thought that it may be a groundbreaking idea that could eliminate diabetes. After hearing your explanation again, I realized that diabetes is different from other diseases.
- *8Vagus nerve: One of the parasympathetic branches of the autonomic nervous system. It branches extensively within the body and is widely distributed.
The secret to building a project team that can deliver results
Nishimura: Finally, although it is not directly related to the research content, I would like to ask you if there is anything that you feel is important regarding management of a team. When looking at the Moonshot Project team, one notable characteristic is the outstanding lineup of team members. I am particularly interested in your team because it is quite large.
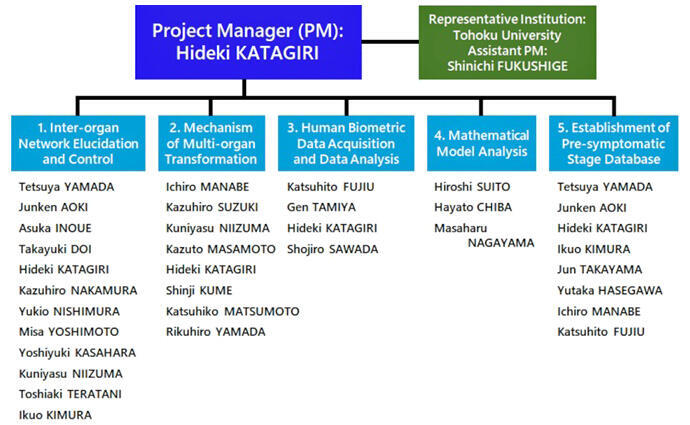
Katagiri: First, the Moonshot Goal 2 has the aim of "Realization of ultra-early disease prediction and intervention by 2050," and my project has 26 teams working on it. My policy has remained the same since I was leading a project on the theme of "aging." I have told the project members, "Everyone, please do what you want to do." I believe that it is best to let them pursue the things they want to, because researchers are people who live for what they want to do.
If they are forced to do something, they may indeed get it done, but their true potential will not be demonstrated. Therefore, to get the most out of them, I want them to work on what they really want to do. This means that it is important to have them hold a sincere desire to do what I would like them to do.
The project on aging involved 18 teams, including both researchers who specialized in aging and individuals like myself who were not experts in the field. We put our utmost effort into making everyone think, "It is interesting to work on the theme of aging."
Ise: What exactly does this policy look like in action?
Katagiri: Instead of forcing them by saying, "Your research field fits into this piece of the aging project, so please work on it," all the members will discuss together, saying things like, "This point seems interesting." By doing so, since everyone is a first-class researcher, proposals will naturally emerge from each individual's perspective such as, "From the viewpoint of my field, we may be able to do something like this." The most important thing is for the researchers themselves to be interested in the project. As is the case with this diabetes project, I think that the main theme of overcoming diabetes is probably interesting and meaningful for everyone. I hope that we can encourage them to pursue their research with the desire to do so while seeking consensus.
Nishimura: I think this is a very sensible approach for every researcher participating in the project to demonstrate their abilities. The fact that you naturally embody this approach is truly remarkable.
Katagiri: We have incredibly talented individuals participating in the project, so I think that we should respect them and encourage them to unleash their full potential.
Nishimura: I completely understand your point. I was frankly impressed by your ability to manage a team as a researcher, as well as the fact that you embody your aspirations, which you had since high school, such as "being involved with human life" and "being of service to society," both as a researcher and as a physician. Thank you very much for your time today.
I felt that Professor Katagiri's path as a physician and researcher, which has been greatly influenced by his encounters with a number of mentors, reflects his humanity and charm. As his research progresses, modern diseases such as diabetes and obesity, which can affect anyone, may be eradicated from the world.
I was filled with emotion as I thought of Professor Katagiri in his high school days, wondering if there could be any better service to society than what he has accomplished so far.

Profile
Hideki Katagiri
Tohoku University Graduate School of Medicine
After working as a medical fellow at the Third Department of Internal Medicine at the University of Tokyo and an assistant professor at the Department of Diabetes and Metabolism at Tohoku University Hospital, he became a Professor at the Centers for Translational and Advanced Research at the Graduate School of Medicine at Tohoku University in 2003. He has been a Professor at the Department of Diabetes, Metabolism and Endocrinology, Tohoku University Graduate School of Medicine since 2013. He also serves as the Vice Dean of the Tohoku University Graduate School of Medicine, Director of the United Centers for Advanced Research and Translational Medicine, and Director of the Department of Diabetes, Metabolism and Endocrinology at Tohoku University Hospital. He received the JSPS Prize and the Prize for Science and Technology, The Commendation by the Minister of Education, Culture, Sports, Science and Technology for his discovery of inter-organ communication networks. He is currently conducting research on a cure for diabetes mellitus as a Project Manager of the Cabinet Office's Moonshot Research & Development Program.
This article was produced in cooperation with the Moonshot Research and Development Project Division of JST.
https://www.jst.go.jp/moonshot/en/index.html
Original article provided by esse-sense and translated by Science Japan.