A simulation model to rationally determine the quarantine duration of patients with mpox (formerly known as monkeypox), an infectious disease of which worldwide spread is concerned, has been developed. The group having conducted the development includes Professor Shingo Iwami, who studies Mathematical Science at the Graduate School of Science at Nagoya University and Scientific Researcher Fuminari Miura, (Theoretical Epidemiology) of the Center for Infectious Disease Control at the National Institute for Public Health and the Environment (RIVM), in the Netherlands. Appropriate isolation durations can be determined by obtaining data on the amount of virus shed by infected persons and its time course, running a simulation, and setting how stringently infection transmission will be contained. The model may be useful in shortening the unnecessary isolation period during which patients have minimal risk of transmitting the virus to others.
Provided by the National Institute of Infectious Diseases
African rodents as the main route of infection
According to Dr. Masahiro Ishikane (Clinical Infectious Diseases) of the Disease Control and Prevention Center at the National Center for Global Health and Medicine, who participated in the research from a clinical perspective, mpox is an infectious disease caused by the DNA virus monkeypox (mpox virus), a species of the genus Orthopoxvirus. Usually, rashes appear with fever and other symptoms after an incubation period of 6-13 days. The disease resolves spontaneously in 2-4 weeks in most cases, but patients with compromised immune systems and elderly patients are at high risk for aggravation of the symptoms.
In 1958, the first report of mpox in mammalians described a smallpox-like infection among laboratory crab-eating macaques at a serology institute in Copenhagen, Denmark, and called the disease "monkeypox." However, rodents such as squirrels and mice that live in Africa are mainly responsible for human infection. The name under the Infectious Diseases Act was changed to "mpox" in May 2023.
World Health Organization (WHO) declares another state of emergency in August
The virus is classified into two subtypes according to genetic differences: the Congo Basin type (Clade I) and the West African type (Clades IIa and IIb). Mpox infection in humans was first confirmed in Zaire (now the Democratic Republic of the Congo) in 1970. In 2022, there was a wave of reports of infected cases, mainly in Europe and the United States. The World Health Organization (WHO) declared a "public health emergency of international concern" on July 23 of the same year.
The first case in Japan was confirmed on the 25th of the same month, and about 200 people were infected by the end of the state of emergency less than a year later. Currently, a genetically distinct group called "Clade Ib" is spreading in the Democratic Republic of the Congo in central Africa. On August 14 of this year, WHO again declared a state of emergency due to the possible risk for spread of the disease outside Africa. As of September 24, 2024, Clade Ib-infected patients have also been reported outside of Africa among people with a history of travel to Africa from Sweden, Thailand, and India.

The basic route of infection is contact with skin lesions, body fluids, or blood of infected people or animals. The frequency of infection is high through contact with mucous membranes, such as sexual intercourse. Even in the absence of direct contact, the possibility of droplet infection has been reported among people who were in conditions similar to "those used to define close contact" during the coronavirus disease 2019 pandemic, i.e., in close proximity to infected persons and exposed to droplets for a long period of time. There have been reports of the virus being detected in the air of infected patients' hospital rooms; however, no actual cases of airborne transmission have been confirmed yet.
Individual differences in the duration of viral shedding
As an infection control precaution, the U. S. Centers for Disease Control and Prevention (CDC) recommends quarantining infected individuals for approximately 3 weeks until the skin lesions improve. Iwami of Nagoya University and his colleagues became interested in "verifying if the length of the isolation period was too short or unnecessarily too long." They decided to build a simulation model with Miura of the RIVM and his colleagues as experts in epidemiology.
For the simulation, they used data from 90 patients in Europe for whom certain information on the duration and amount of viral shedding was available from papers and other sources. The duration until an infected person tested negative for the virus by PCR and was considered to be no longer shedding the virus was estimated to range from 23 to 50 days. However, principal component analysis showed that the 90 patients fell into two groups: "infected individuals with low transmission risk" (71 individuals) and "infected individuals with high transmission risk" (19 individuals). The mean duration of viral shedding was 30.1 days in the former group and 42.7 days in the latter group. The analysis results indicate that the duration of viral shedding varies greatly from an infected individual to another.

Provided by Professor Shingo Iwami of Nagoya University
Prevention of transmission tested with three rules
The group examined different rules for ending the isolation in terms of the effectiveness in preventing transmission and the length of unnecessary isolation during which individuals posed no risk of transmitting the virus to other people. These three rules were: (1) ending the isolation after the disappearance of symptoms such as rash, (2) ending the isolation after a fixed duration (approximately 3 weeks), and (3) ending the isolation after a specified number of negative test results. Simulations were conducted using the assumptions, including: a virus concentration of 1 million copies or more per milliliter in a lesion or other sites of an infected person exceeds the "infectiousness threshold" and poses a risk for transmission to others; and the setting that the acceptable risk of premature termination of isolation is less than 5%. The results showed minimized unnecessary isolation periods of 15.1 days for (1), 9.4 days for (2), and 7.4 days for (3) if negative results in three consecutive PCR tests at 5-day intervals were required to end the isolation.
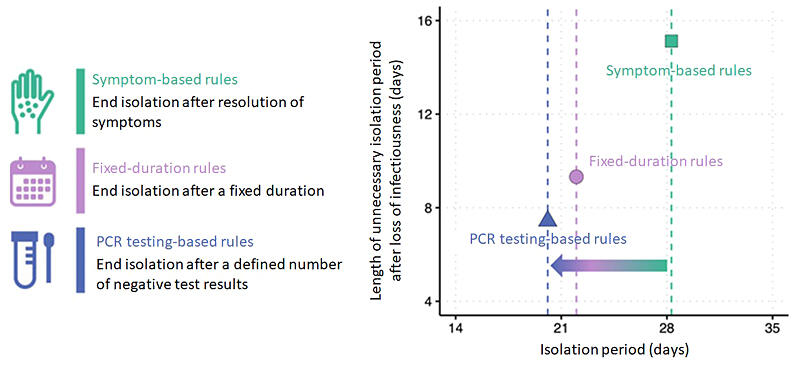
Provided by Professor Shingo Iwami of Nagoya University
Findings may contribute to the establishment of global guidelines
The mpox virus variant assumed in this simulation was Clade IIb, which was prevalent in 2022. Currently, the declaration of emergency assumes the Clade Ib virus, which is considered to have a higher fatality rate than Clade IIb. Nevertheless, the infectivity and effectiveness of the vaccine being prepared are not yet well understood.
The available data are insufficient to validate the duration and other aspects of isolation for Clade Ib with the model developed in this study. However, Iwami says, "Our model may contribute to the validation of the isolation criteria adopted by each country based on clinical and epidemiological data and empirical rules, and establishment of flexible, globally applicable isolation guidelines based on mathematical models."
The study was conducted jointly by Nagoya University, Kyushu University, Kyoto University, and other institutions with support from the Moonshot Research and Development Program and Strategic Basic Research Program of Japan Science and Technology Agency (JST). The results were published in the British online science journal Nature Communications on August 26.
(NAGASAKI Midoriko / Science Portal Editorial Office)
Original article was provided by the Science Portal and has been translated by Science Japan.